The Brain Can Adapt, After a Stroke
During and right after a stroke, everyone is praying and hoping for survival. They (I) survived, but what are the challenges? How bad is it? What are we going to do now? The dueling emotions begin. Will I (they) get better? How long will it take?
A few months down the road…
WTF, why am I (they) not better? The stroke patient probably is better, but they are not back to pre-stroke functioning. That is when the stress and pressure come to get back to pre-stroke level functioning. The frustration, anger, and giving up stages may occur. This happens to stroke survivors, their partners, and their families.
Stroke survivors can improve if they keep doing the exercises and working even when they do not see anything improving. The small improvements will help, keep after it. Very few stroke survivors get back to pre-stroke functioning. The sooner you realize that the sooner you can begin to grieve your losses.
Why would I say that after saying a stroke survivor can keep improving? Because it is true. Stroke survivors can improve and get stronger and better, but they probably will not be back to pre-stroke level. If the pre-stroke level is your ONLY goal, you will be angry, mad, and frustrated for the rest of your life.
What if you set your main goal to be improving as much as you can AND adapting to your normal now? It is great that you keep striving for improvement. What is not great is that you will not accept anything except pre-stroke level functioning. You are setting yourself up for depression and being a difficult person to be around.
Neuroplasticity
Neuroplasticity is the brain’s ability to adapt and change throughout a person’s life. This process is essential for learning and memory, and it is also crucial for recovery after injury or disease. In particular, neuroplasticity plays a significant role in helping patients with dementia and stroke survivors regain lost cognitive and physical abilities.
Dementia is a chronic condition that affects millions of people worldwide. It is characterized by a decline in cognitive function, including memory loss, difficulty with language, and impaired judgment. While there is no cure for dementia, researchers have found that neuroplasticity can help slow the progression of the disease and improve patients’ quality of life. Similarly, stroke survivors often experience physical and cognitive impairments that can be addressed through targeted neuroplasticity-based therapies. By understanding the mechanisms of neuroplasticity, doctors and therapists can develop personalized treatment plans that help patients recover lost abilities and improve their overall well-being.
Basics of Neuroplasticity
Defining Neuroplasticity
Neuroplasticity can be defined as the brain’s ability to change and adapt in response to experience, learning, and injury. This process involves changes in the structure and function of the brain at the level of individual neurons and neural networks. These changes can occur in response to a wide range of stimuli, including sensory input, cognitive and motor activity, and environmental factors.
Mechanisms of Neuroplasticity
Neuroplasticity is how the brain can change and adapt. It happens in a few different ways, like making connections between brain cells stronger, growing new brain cells and connections, and changing how our genes work. One important way the brain can change is called synaptic plasticity, which is all about how strong and how many connections there are between brain cells. This is important for learning and remembering things, and for getting better after a brain injury.
Another important mechanism of neuroplasticity is neurogenesis, which refers to the growth of new neurons in the brain. This process occurs primarily in the hippocampus, a region of the brain that is critical for learning and memory. Neurogenesis is thought to play an important role in the recovery of function after brain injury, as well as in the development of new treatments for dementia and other neurological disorders.
Dementia Overview
Understanding Dementia
Dementia is a term used to describe a group of symptoms that affect memory, thinking, and social abilities, to the extent that it interferes with daily life. It is a progressive disease that affects the brain, causing a decline in cognitive function. Dementia can be caused by a variety of factors, including genetics, lifestyle, and environmental factors.
Types of Dementia
There are several types of dementia, each with its own unique set of symptoms and causes. The most common type of dementia is Alzheimer’s disease, which accounts for 60-80% of all dementia cases. Other types of dementia include vascular dementia, Lewy body dementia, frontotemporal dementia, and mixed dementia.
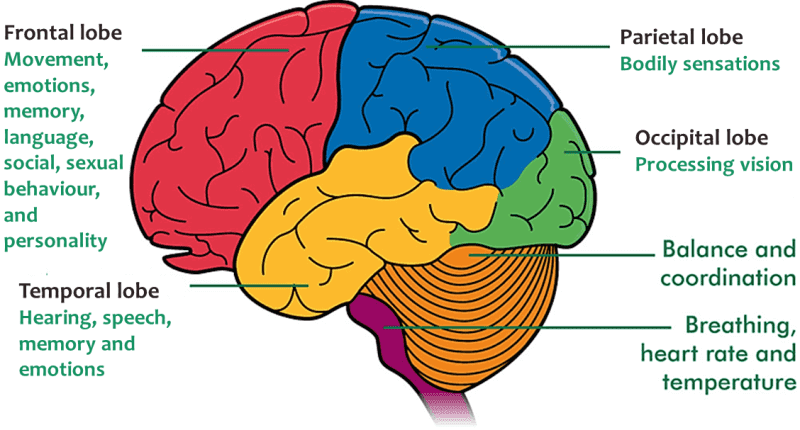
In Alzheimer’s disease, the brain cells degenerate and die, causing a steady decline in cognitive function. Vascular dementia is caused by a series of small strokes that damage the brain. Lewy body dementia is caused by the abnormal buildup of proteins in the brain, while frontotemporal dementia is caused by the degeneration of the frontal and temporal lobes of the brain. Mixed dementia is a combination of two or more types of dementia.
Understanding the type of dementia a patient has is important in determining the appropriate treatment plan. While there is currently no cure for dementia, there are medications and therapies available to help manage symptoms and improve quality of life.
In stroke survivors, neuroplasticity can help promote recovery by facilitating functional changes in the brain. Stroke disturbs both the structural and functional integrity of the brain, but harnessing neuroplasticity can help promote substantial and enduring improvements in long-term outcomes for stroke survivors.
Stroke Fundamentals
Defining Stroke
A stroke is a medical emergency that occurs when blood flow to the brain is disrupted, resulting in brain damage. The damage can be temporary or permanent, depending on the severity of the stroke and how quickly it is treated. According to the American Stroke Association, stroke is the fifth leading cause of death in the United States, and it is a leading cause of serious long-term disability.
Types of Stroke
There are two main types of stroke: ischemic stroke and hemorrhagic stroke. Ischemic stroke occurs when a blood clot blocks a blood vessel in the brain. Hemorrhagic stroke occurs when a blood vessel in the brain ruptures and bleeds into the brain tissue.
Ischemic stroke is the most common type of stroke, accounting for about 87% of all strokes. Hemorrhagic stroke is less common, accounting for about 13% of all strokes. However, hemorrhagic stroke is more deadly than ischemic stroke, with a higher risk of death and disability.
Risk factors for stroke include high blood pressure, smoking, diabetes, high cholesterol, and a family history of stroke. It is important to manage these risk factors to prevent stroke.
Neuroplasticity in Dementia Patients
Neuroplasticity refers to the brain’s ability to reorganize itself by forming new neural connections throughout life. This ability plays a crucial role in learning, memory, and recovery from brain injury. In dementia patients, neuroplasticity can help compensate for the loss of brain cells and function, allowing the individual to adapt to new situations and maintain some level of independence.
Adaptation and Compensation
Dementia patients often experience a decline in cognitive function, including memory, attention, and language skills. However, research has shown that the brain can adapt to these changes by recruiting other areas to perform these functions. For example, if a patient with dementia has difficulty with language, other areas of the brain may take over this function, allowing the individual to communicate effectively.
In addition, neuroplasticity can help dementia patients compensate for their cognitive deficits by developing new strategies for completing tasks. For example, a patient with memory loss may learn to use a calendar or notes to remember important information.
Challenges and Limitations
While neuroplasticity can be beneficial for dementia patients, it is important to note that this ability may be limited in individuals with advanced dementia. In addition, the brain’s ability to adapt may be affected by other factors, such as age, overall health, and the severity of the dementia.
Furthermore, neuroplasticity may not always lead to positive outcomes. For example, in some cases, the brain may compensate for cognitive deficits by relying on less efficient neural pathways, which can lead to further cognitive decline over time.
Overall, while neuroplasticity offers potential benefits for dementia patients, it is important to consider the individual’s specific needs and limitations when developing treatment plans. Caregivers and healthcare professionals can work together to identify strategies that promote neuroplasticity and improve the quality of life for individuals with dementia.
Neuroplasticity in Stroke Survivors
Recovery and Rehabilitation
After a stroke, the brain undergoes a series of changes in an attempt to compensate for the damage caused by the stroke. This process is known as neuroplasticity. The brain’s ability to reorganize itself and form new neural connections is key to recovery and rehabilitation after a stroke.
Rehabilitation programs for stroke survivors aim to take advantage of the brain’s plasticity by providing intensive therapy that promotes the formation of new neural connections. This therapy can include physical therapy to improve motor function, speech therapy to improve communication, and cognitive therapy to improve memory and other cognitive abilities.
Strategies for Enhancing Plasticity
There are a number of strategies that can be used to enhance neuroplasticity in stroke survivors. One approach is to use repetitive training to promote the formation of new neural connections. This can involve practicing a specific task or movement over and over again until it becomes automatic.
Another approach is to use non-invasive brain stimulation techniques, such as transcranial magnetic stimulation (TMS) or transcranial direct current stimulation (tDCS), to stimulate the brain and promote the formation of new neural connections.
Finally, engaging in activities that challenge the brain, such as learning a new language or musical instrument, can also promote neuroplasticity and aid in stroke recovery.
While the brain’s ability to reorganize itself and form new neural connections is critical to recovery and rehabilitation after a stroke, it is important to note that the extent of neuroplasticity varies from person to person. Some individuals may have a greater capacity for neuroplasticity than others, and the success of rehabilitation programs may depend on a variety of factors, including the severity of the stroke and the individual’s overall health.
Comparative Analysis
Differences in Neuroplastic Responses
Dementia and stroke are two distinct neurological conditions that affect the brain in different ways. Dementia is a progressive disorder that affects memory, thinking, and behavior, while stroke is a sudden interruption of blood flow to the brain, which can cause damage to brain cells. As a result, the neuroplastic responses of dementia patients and stroke survivors differ significantly.
In dementia patients, the neuroplastic responses are impaired due to the progressive nature of the disease. The brain’s ability to reorganize and adapt to new situations is reduced, and the formation of new neural connections is limited. This is due to the degeneration of brain cells and the accumulation of toxic proteins that interfere with the brain’s normal functioning.
In contrast, stroke survivors experience a sudden loss of brain function, which triggers a neuroplastic response aimed at restoring lost functions. The brain’s ability to reorganize and adapt to new situations is enhanced, and the formation of new neural connections is encouraged. This is due to the brain’s ability to compensate for the loss of function by activating other regions of the brain that were previously not used.
Similarities in Neuroplastic Adaptations
Despite the differences in neuroplastic responses, dementia patients and stroke survivors share some similarities in their neuroplastic adaptations. Both conditions result in changes to the brain’s structure and function, which can lead to the formation of new neural connections. This is due to the brain’s ability to adapt to new situations and to compensate for lost functions.
In both cases, neuroplastic adaptations can be enhanced through targeted rehabilitation programs that focus on stimulating the brain and promoting the formation of new neural connections. These programs can include cognitive and physical exercises, as well as other forms of therapy that encourage the brain’s natural ability to reorganize and adapt to new situations.
Overall, while the neuroplastic responses of dementia patients and stroke survivors differ significantly, both conditions share some similarities in their neuroplastic adaptations. By understanding these similarities and differences, healthcare professionals can develop more effective rehabilitation programs that take into account the unique needs of each patient.
Therapeutic Interventions
Neuroplasticity is the ability of the brain to change and adapt in response to external stimulation or damage. Therapeutic interventions can help promote neuroplasticity in dementia patients and stroke survivors, enhancing their cognitive and physical abilities.
Cognitive Therapy
Cognitive therapy is a form of therapy that focuses on improving cognitive abilities such as memory, attention, and problem-solving. It is an effective intervention for dementia patients and stroke survivors, as it can help improve their cognitive abilities and promote neuroplasticity.
One example of cognitive therapy is cognitive stimulation therapy (CST), which involves engaging patients in structured activities designed to stimulate their cognitive abilities. CST has been shown to improve cognitive function and quality of life in dementia patients [1].
Physical and Occupational Therapy
Physical and occupational therapy are interventions that focus on improving physical abilities such as strength, balance, and coordination. They are effective interventions for stroke survivors, as they can help improve physical function and promote neuroplasticity.
Physical therapy involves exercises and activities designed to improve strength, balance, and coordination. Occupational therapy involves activities designed to improve daily living skills such as bathing, dressing, and cooking.
One example of physical therapy is constraint-induced movement therapy (CIMT), which involves restricting the use of the unaffected limb to encourage the use of the affected limb. CIMT has been shown to improve motor function and promote neuroplasticity in stroke survivors [2].
In conclusion, therapeutic interventions such as cognitive therapy and physical and occupational therapy can be effective in promoting neuroplasticity in dementia patients and stroke survivors. These interventions can improve cognitive and physical function, and enhance quality of life for those affected by these conditions.
[1] Spector, A., Thorgrimsen, L., Woods, B., Royan, L., Davies, S., Butterworth, M., & Orrell, M. (2003). Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial. The British Journal of Psychiatry, 183(3), 248-254.
[2] Taub, E., Miller, N. E., Novack, T. A., Cook, E. W., Fleming, W. C., Nepomuceno, C. S., … & Crago, J. E. (1993). Technique to improve chronic motor deficit after stroke. Archives of physical medicine and rehabilitation, 74(4), 347-354.
Future Directions in Research
Innovations in Treatment
Research in neuroplasticity has shown promising results in the treatment of dementia and stroke survivors. However, there is still a long way to go before these treatments become widely available. Future research should focus on developing innovative treatment options that can be easily accessible to patients.
One promising area of research is the use of virtual reality (VR) technology in neurorehabilitation. VR can provide patients with a safe and controlled environment to practice real-world activities, which can help improve their cognitive and motor skills. Studies have shown that VR-based rehabilitation can be effective in improving balance, gait, and overall functional ability in stroke survivors and dementia patients [1].
Another area of innovation is the use of non-invasive brain stimulation techniques such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS). These techniques can modulate neural activity in specific brain regions, which can help improve cognitive and motor function in stroke survivors and dementia patients [2].
Predictive Biomarkers
Identifying biomarkers that can predict the progression of dementia and stroke can help clinicians develop personalized treatment plans for patients. Recent studies have shown that certain genetic and epigenetic markers can predict the risk of dementia and stroke [3].
One promising area of research is the use of neuroimaging techniques such as magnetic resonance imaging (MRI) and positron emission tomography (PET) to identify biomarkers of neuroplasticity. These techniques can help identify changes in brain structure and function that are associated with neuroplasticity. By identifying these biomarkers, clinicians can develop targeted interventions that can help improve neuroplasticity in dementia and stroke patients.
In conclusion, future research in neuroplasticity should focus on developing innovative treatment options that are easily accessible to patients and identifying predictive biomarkers that can help clinicians develop personalized treatment plans for patients.
References:
- Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017 Nov 20;11(11).
- Lefaucheur JP. A comprehensive database of published tDCS clinical trials (2005-2016). Neurophysiol Clin. 2016 Nov;46(4-5):319-398.
- Kunkle BW, Grenier-Boley B, Sims R, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat Genet. 2019 Mar;51(3):414-430.
Frequently Asked Questions
How does neuroplasticity contribute to recovery in stroke survivors?
Neuroplasticity is the brain’s ability to adapt and change in response to new experiences and learning. After a stroke, the brain undergoes structural and functional changes that can lead to recovery. Neuroplasticity plays a crucial role in this recovery process by allowing the brain to form new connections between neurons and reorganize neural networks. This rewiring of the brain can help to compensate for damaged areas and improve motor function, language ability, and cognitive function.
What techniques are used to enhance neuroplasticity during stroke rehabilitation?
There are several techniques used to enhance neuroplasticity during stroke rehabilitation. These techniques include constraint-induced movement therapy, mental practice, and repetitive task training. Constraint-induced movement therapy involves restricting the use of the unaffected limb to force the use of the affected limb. Mental practice involves imagining performing a task to activate the same neural networks involved in the actual task. Repetitive task training involves repeating a task to strengthen neural connections and improve motor function.
Can neuroplasticity be harnessed to improve cognitive function in dementia patients?
Yes, neuroplasticity can be harnessed to improve cognitive function in dementia patients. Research has shown that cognitive training, physical exercise, and social engagement can all promote neuroplasticity and improve cognitive function in dementia patients. These interventions can help to strengthen existing neural connections and form new connections, leading to improvements in memory, attention, and executive function.
What is the timeline for neuroplastic changes following a stroke?
The timeline for neuroplastic changes following a stroke varies depending on the severity of the stroke and the individual’s age and overall health. In general, the brain undergoes the most significant changes in the first few months following a stroke. However, neuroplastic changes can occur throughout a person’s lifetime, and ongoing rehabilitation and therapy can continue to promote recovery.
How do brain cells regenerate and adapt after a stroke?
After a stroke, brain cells can regenerate and adapt through several processes, including neurogenesis, synaptogenesis, and angiogenesis. Neurogenesis involves the formation of new neurons, while synaptogenesis involves the formation of new connections between neurons. Angiogenesis involves the growth of new blood vessels, which can help to provide oxygen and nutrients to damaged areas of the brain. These processes can help to repair damaged neural networks and improve function.
What is the relationship between neuroplasticity and the risk of dementia post-stroke?
Research has shown that neuroplasticity can play a protective role in reducing the risk of dementia post-stroke. By promoting the formation of new neural connections and strengthening existing connections, neuroplasticity can help to compensate for the damage caused by the stroke and reduce the risk of cognitive decline. Ongoing rehabilitation and therapy can continue to promote neuroplasticity and reduce the risk of dementia post-stroke.


