You get the information about the stroke and what has happened. Probably, how to help prevent it in the future, but, how often do your questions get answered? What about the questions that you have that you don’t ask?
Thoughts are racing around inside your head. Questions, so many questions are popping up, too. You are afraid to ask some of them. Hey, that is completely normal. You have just survived a stroke and things have changed and you don’t know what is permanent, what will improve or even how long it will take. Now, would be a really good time to start journaling to get those thoughts out of your head. If you can’t write, you can speak into a recording device or even your phone. Supressing them and ruminating on them will only make you feel worse.
This isn’t the time to solve your questions or concerns, it is ktime to get them out of your head. You probably are not in any shape mentally, to make good decisions. Give yourself a little time and grace. None of us make good decisions when we are stressed.
What Stroke Survivors Face
Stroke survivors face a multitude of challenges in their road to recovery. They often require education on post-stroke physical changes, computer proficiency, driving, motivation, and practical help from others. While many stroke survivors receive some form of rehabilitation and support, there is a growing need for more comprehensive care that addresses the unique needs of stroke survivors.
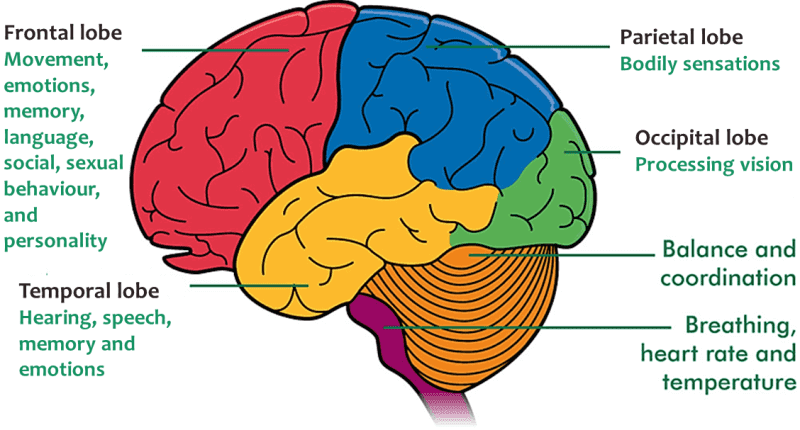
Many stroke survivors experience physical changes such as weakness, numbness, and difficulty with balance and coordination. Rehabilitation can help address these issues, but ongoing education and support are necessary to ensure that stroke survivors can continue to make progress.
Computer proficiency is also crucial for stroke survivors, as technology is an increasingly important part of daily life. Many stroke survivors struggle with using computers and other devices due to physical limitations or cognitive impairments. Education and support in this area can help stroke survivors stay connected with loved ones, access important information, and even find new job opportunities.
Understanding Post-Stroke Physical Changes
One common physical change after a stroke is muscle weakness. This can affect the survivor’s ability to perform everyday tasks, such as getting dressed or cooking. Physical therapy can help improve muscle strength and function, and occupational therapy can teach the survivor how to adapt to their physical limitations.
Another physical change that stroke survivors may experience is paralysis. This can affect one side of the body or a specific limb. Rehabilitation can help the survivor regain movement and function in the affected area. In some cases, assistive devices such as braces or wheelchairs may be necessary to help the survivor move around.
Stroke survivors may also experience difficulty with coordination and balance. This can make it challenging to walk or perform other activities. Physical therapy can help improve coordination and balance, and occupational therapy can teach the survivor how to perform activities of daily living safely.
Stroke survivors need to work closely with their healthcare team to understand their physical changes and develop a plan for managing them. This may include regular physical therapy and occupational therapy sessions, as well as assistance from family members or caregivers. By understanding their physical changes and learning how to manage them, stroke survivors can improve their quality of life and regain their independence.
Computer Proficiency for Stroke Survivors
After a stroke, many survivors want to learn how to use the computer efficiently. They may need to relearn how to type, use a mouse, or navigate the internet. Fortunately, there are many adaptive technologies available that can help stroke survivors improve their computer skills.
Adaptive Technologies for Stroke Rehabilitation
Adaptive technologies are tools that can help people with disabilities use computers more easily. For example, a person with limited hand mobility may benefit from using a trackball or a touchpad instead of a traditional mouse. Or, a person with vision impairment may benefit from using a screen reader that reads text out loud.
There are also many software programs available that can help stroke survivors improve their cognitive skills. For example, some programs can help improve memory, attention, and problem-solving skills. These programs can be especially helpful for stroke survivors who are experiencing cognitive impairments as a result of their stroke.
Efficiency Tips and Tricks
In addition to using adaptive technologies, there are many tips and tricks that stroke survivors can use to improve their computer efficiency. For example, they can use keyboard shortcuts to perform common tasks more quickly. They can also customize their computer settings to make the text larger or the colors more contrasting, which can be helpful for people with vision impairments.
Another helpful tip is to break tasks down into smaller steps. For example, if a stroke survivor wants to send an email, they can break the task down into smaller steps, such as opening their email program, composing the email, and sending it. This can make the task feel less overwhelming and more manageable.
Overall, it is important for stroke survivors to have access to computer training and adaptive technologies to help them improve their computer skills. By using these tools and techniques, they can become more efficient and independent in their daily lives.
Driving After a Stroke
After a stroke, driving can be a concern for stroke survivors. Some stroke survivors may experience physical changes that can impact their ability to drive safely. However, with proper assessment, training, and vehicle modifications, many stroke survivors can resume driving.
Assessment and Training
It is important for stroke survivors to undergo an assessment by a healthcare professional before resuming driving. The assessment may include a physical examination, vision test, and cognitive evaluation. The healthcare professional will offer a professional opinion about how the stroke might change the ability to drive.
If the healthcare professional determines that the stroke survivor is fit to drive, they may recommend driver training to improve driving skills. Driver training may include on-road instruction, classroom instruction, and computer-based training.
Vehicle Modifications
Vehicle modifications can help stroke survivors drive more safely. Some common vehicle modifications include:
- Hand controls: Hand controls allow stroke survivors to operate the accelerator and brake pedals with their hands instead of their feet.
- Steering wheel modifications: Steering wheel modifications can make it easier for stroke survivors to turn the wheel and maintain control of the vehicle.
- Seat modifications: Seat modifications can help stroke survivors sit more comfortably and maintain good posture while driving.
It is important for stroke survivors to work with a qualified professional to determine which vehicle modifications are necessary and to ensure that the modifications are installed correctly.
Overall, stroke survivors can resume driving with proper assessment, training, and vehicle modifications. Stroke survivors need to work with healthcare professionals and qualified professionals to ensure their safety and the safety of others on the road.
Boosting Motivation in Stroke Rehabilitation and Recovery
Stroke survivors often face a variety of physical, psychological, and social challenges that can impact their motivation to recover. However, several strategies can help boost motivation and improve overall recovery outcomes.
Setting Achievable Goals
One effective way to boost motivation in stroke recovery is to set achievable goals. This can help stroke survivors stay focused and motivated as they work towards specific milestones. Goals should be realistic, measurable, and tailored to the individual’s needs and abilities. For example, a stroke survivor may set a goal to walk a certain distance without assistance or to improve their ability to use their affected arm or hand. One of the hardest things to do must be to keep exercising and working on regaining more use of an affected part of the body when you cannot see much if any, improvement. Decide to keep on working, no matter what you see or don’t see at this moment in time.
Community and Support
Another important factor in boosting motivation is having a strong support system. This can include family members, friends, healthcare providers, and support groups. Having a community of people who understand the challenges of stroke recovery can provide encouragement, motivation, and practical help. Support groups can also provide opportunities for socialization and connection with others who are going through similar experiences.
In addition to community support, stroke survivors may benefit from working with healthcare providers who specialize in stroke rehabilitation. These professionals can provide guidance, education, and practical strategies for improving motivation and achieving recovery goals.
Overall, boosting motivation in stroke recovery is an important aspect of achieving optimal recovery outcomes. By setting achievable goals and building a strong support system, stroke survivors can stay motivated and engaged in their recovery journey.
When motivation fails, discipline prevails. I don’t remember where I saw that, but I believe it to be true. Motivation may come and go but discipline requires effort and it is a choice that each of us must make to either do or not do. Discipline is doing the thing(s) that you said you would do, no matter if you feel like doing it or not.
Practical Assistance for Stroke Survivors
Stroke survivors often require practical assistance to help them adjust to their new life after a stroke. This section will discuss the two main types of practical assistance that stroke survivors may need: home adjustments and caregiver support.
Home Adjustments
After a stroke, it may be necessary to make changes to the home environment to make it more accessible and safe for the stroke survivor. Some common home adjustments include:
- Installing grab bars in the bathroom and shower
- Adding non-slip mats to the bathroom and shower
- Installing handrails on stairs
- Removing obstacles and clutter from walkways
- Widening doorways to accommodate a wheelchair or walker
Making these adjustments can help stroke survivors feel more comfortable and confident in their home environment.
Caregiver Support
Stroke survivors may also require practical help from others, including family members, friends, or professional caregivers. Caregivers can assist with a variety of tasks, such as:
- Preparing meals
- Assisting with personal care, such as bathing and dressing
- Providing transportation to appointments and errands
- Helping with household chores, such as cleaning and laundry
Caregivers can also provide emotional support and motivation to stroke survivors, which can be an important part of the recovery process.
Overall, stroke survivors require practical assistance to help them adjust to their new life after a stroke. By making home adjustments and receiving caregiver support, stroke survivors can maintain their independence and improve their quality of life.
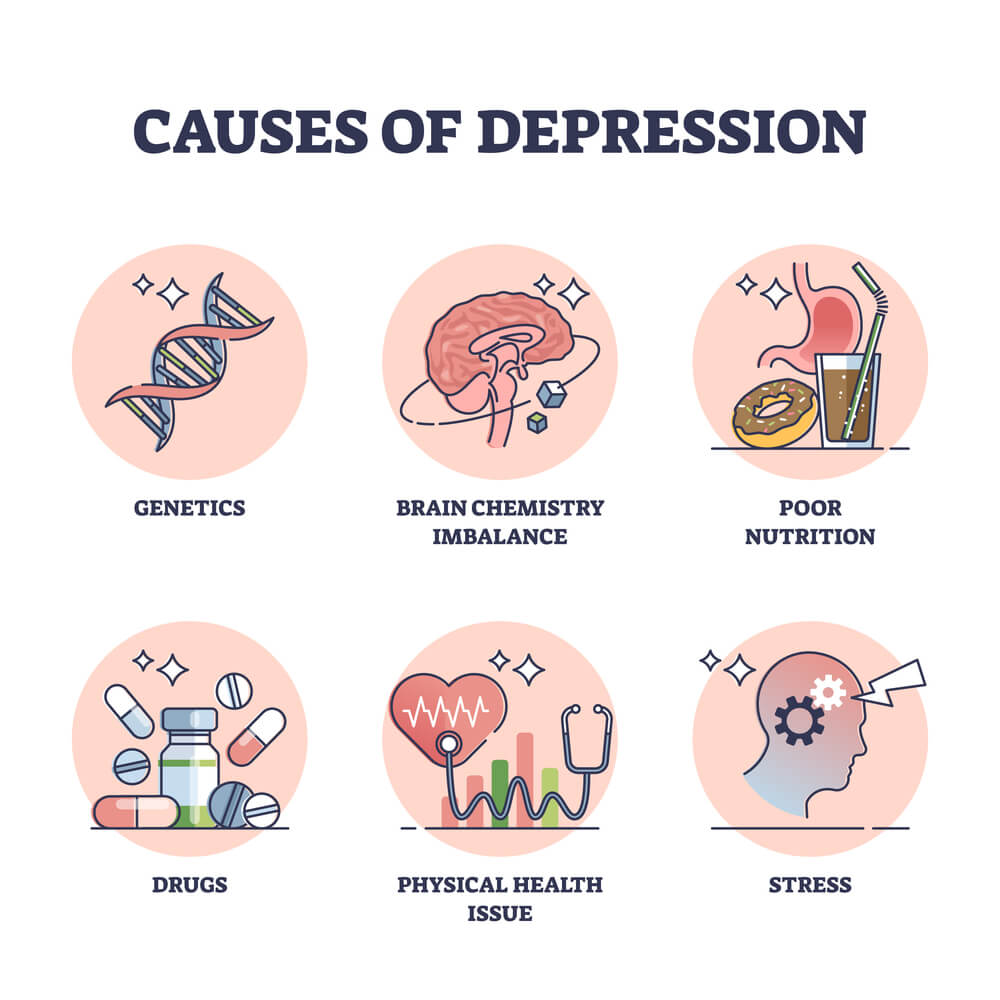
Health Management and Secondary Prevention
After a stroke, survivors may experience a range of physical changes that can affect their daily lives. These changes may include difficulty with movement, speech, and cognition. According to a recent study, stroke survivors want more education about post-stroke physical changes, including how to manage their symptoms and improve their overall health [1].
In addition to physical changes, stroke survivors may also need help with practical tasks, such as using the computer efficiently, driving, and improving their motivation. Stroke survivors need to have access to resources that can help them manage their health and prevent future strokes.
One key aspect of health management and secondary prevention for stroke survivors is education about lifestyle changes that can reduce the risk of future strokes. These changes may include managing blood pressure, maintaining a healthy weight, quitting smoking, and getting regular exercise [2].
Another important aspect of health management and secondary prevention is access to support from others. Stroke survivors may benefit from working with a physical therapist, occupational therapist, or speech therapist to improve their physical function and communication skills. Additionally, support from family members, friends, and other stroke survivors can be helpful in managing the emotional and practical challenges of life after a stroke [3].
Overall, stroke survivors need access to a range of resources to help them manage their health and prevent future strokes. These resources may include education about lifestyle changes, practical support with daily tasks, and emotional support from others. By working with healthcare providers, family members, and other stroke survivors, stroke survivors can take steps to improve their health and quality of life after stroke.
[2] “Preventing Another Stroke | American Stroke Association”
Reintegration into Community and Work
Stroke survivors often face challenges when reintegrating into their communities and workplaces. They may experience physical changes that affect their daily activities, such as difficulty using their hands or walking. In a study by BMC Neurology, it was found that survivors want more education on post-stroke physical changes and how to improve their motivation.
In addition, many stroke survivors require practical help from others to reintegrate into their communities. For example, they may need assistance with driving, using the computer efficiently, or finding employment. It is important for stroke survivors to have access to resources that can help them with these tasks.
One way to provide support to stroke survivors is through community-based interventions. According to a study by PubMed, community-based interventions can facilitate the necessary support for stroke survivors, caregivers, families, and communities to optimize stroke recovery. These interventions can include education and training programs, support groups, and access to healthcare services.
Overall, stroke survivors need access to resources and support to successfully reintegrate into their communities and workplaces. By providing education, practical help, and community-based interventions, stroke survivors can improve their quality of life and achieve their goals.
Frequently Asked Questions
What adaptive technologies can assist with computer use after a stroke?
Stroke survivors may experience difficulty with computer use due to physical or cognitive impairments. Adaptive technologies can help individuals overcome these challenges. For example, voice recognition software can be used to control the computer with voice commands, while a trackball or touchpad can be used instead of a traditional mouse. Other adaptive technologies include ergonomic keyboards, screen magnifiers, and speech-to-text software.
How can stroke survivors relearn to drive safely and regain independence?
Driving is an important aspect of independence for many stroke survivors. However, it is important to ensure that the individual is physically and cognitively ready to drive safely. Rehabilitation programs can help stroke survivors regain the skills needed for safe driving. Adaptive equipment, such as hand controls or left-foot accelerators, may also be necessary. It is important to consult with a healthcare professional before returning to driving after a stroke.
What types of physical exercises are recommended for stroke rehabilitation?
Physical exercise is an important part of stroke rehabilitation. The type and intensity of exercise will depend on the individual’s specific needs and abilities. Common exercises include range-of-motion exercises, strength training, and aerobic exercise. Rehabilitation programs may also include activities such as gait training, balance training, and functional training.
In what ways can stroke survivors boost their motivation during recovery?
Motivation can be a challenge during stroke recovery. Setting achievable goals and celebrating small successes can help boost motivation. Engaging in enjoyable activities and spending time with supportive friends and family members can also be helpful. Joining a support group or working with a counselor can provide additional motivation and emotional support.
What resources are available to educate stroke survivors and their families about post-stroke life?
There are many resources available to educate stroke survivors and their families about post-stroke life. The American Stroke Association provides a range of resources, including educational materials and support groups. Rehabilitation centers and healthcare providers can also provide information and resources. Online resources, such as blogs and forums, can also be helpful.
How can the community provide practical support to individuals recovering from a stroke?
The community can play an important role in supporting individuals recovering from a stroke. Simple acts of kindness, such as offering to run errands or providing transportation, can be helpful. Community organizations, such as churches or volunteer groups, may also provide practical support. It is important to communicate with the individual and ask how they would like to be supported.