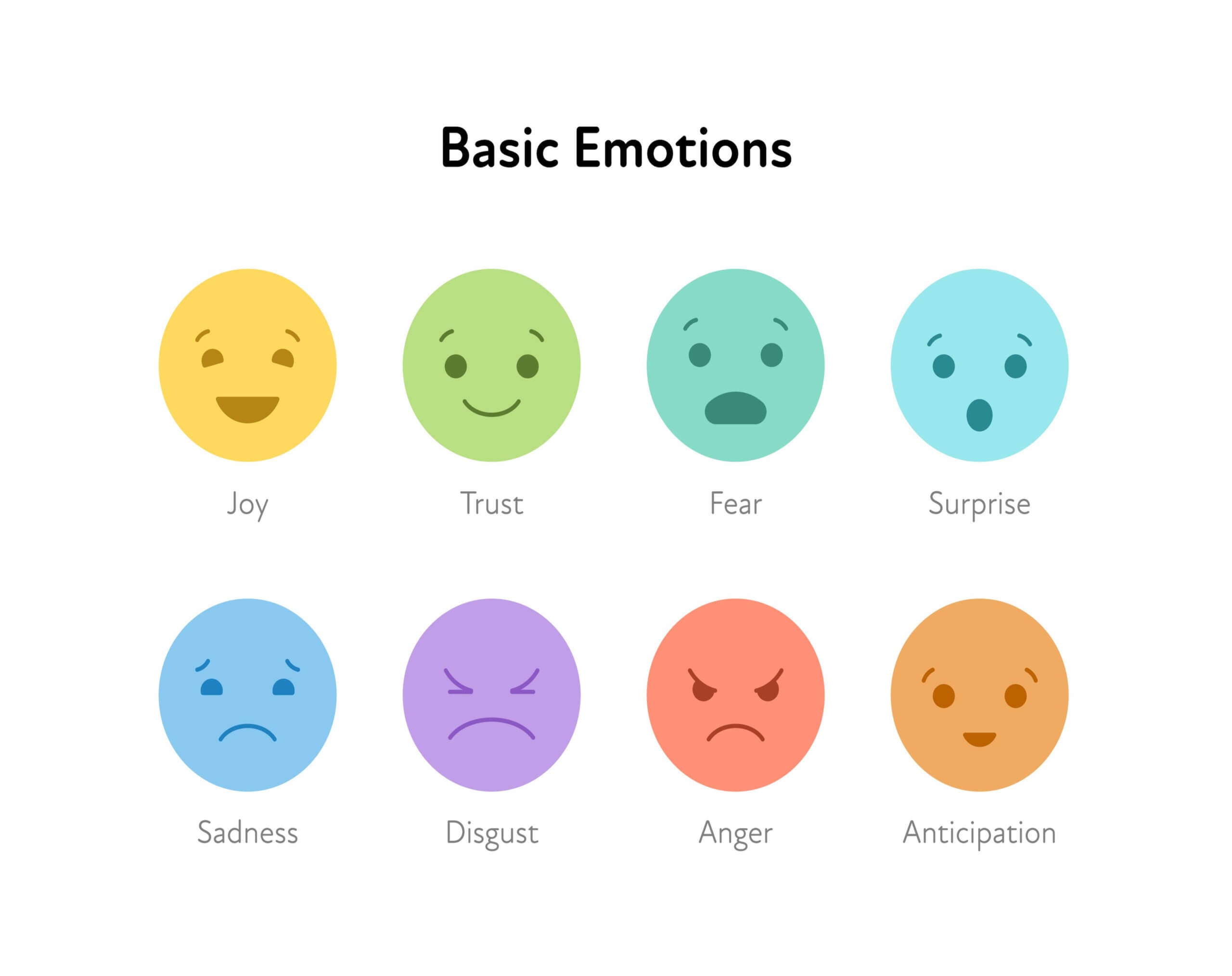
You may try stuffing negative emotions down, or you may just ignore them … it will work, for a while. Then watch out! They will come out and it rarely will be in a productive way. Recognize them. Acknowledge them. The emotions you are feeling are valid.
June 29, 2022
Of course, you love them and want to help them. You think that because you love them and you want to help them, everything will be okay. It won’t. Dueling emotions and feelings will arise. It usually becomes overwhelming in a few short months.
Accepting what you feel
Be healthier. Be more on top of things. Be accepting of what and how you feel. It is okay to feel resentful sometimes. It is okay to feel lonesome. It is okay to feel angry at your loved one’s frustrating behavior. You will have some thoughts and feelings that you will feel guilty over. Sadness will creep in. You will probably start grieving for them a little while after the diagnosis.
It takes a lot of energy and effort to hold in your feelings. Stifling your feelings and emotions can cause high stress, sudden angry outbursts, unhealthy life choices, problems sleeping, increased risk of depression and hopelessness.
Give yourself permission to vent
Will you give yourself permission to say what and how you are feeling? You need a trusted person that will listen to you and not judge. You do need to vent. You may also need to tell the person that you are talking with that you just need to vent. You are not looking for solutions or suggestions. This is where support groups can help, too.
Don’t feel guilty about your feelings.
That is always easier said than done. Do you have unrealistic expectations? Do you beat yourself up over negative emotions? It is okay to get mad. For example, your loved one has made a huge mess with the meal. It is at the end of the day and you are tired because it has been a very tough day. Now, you have to clean up the mess. You have to get your loved one cleaned up and changed.
The problem isn’t that you have negative feelings
The problem is not that you have unpleasant feelings, the problems arise when you haven’t taken care of them and you hurt yourself physically or emotionally or you hurt your care receiver physically or emotionally. You don’t bottle them up and you don’t let loose in front of your loved one. What will be your safe outlet? Take care of the mess and your loved one, then find your ways to decompress.
Suggestions:
-
- Call or text with a supportive friend, family member or another caregiver
-
- Go to a support group meeting
-
- Cry
-
- Go for a run or walk
-
- Journal – let it free flow and write whatever comes up
-
- Find a punching bag (a real one or a pillow) to punch, throw or scream into
-
- Cleaning
-
- Take a break, call in reinforcements
-
- Take a hot shower or soak in a bath
-
- Watch a TV show or a movie
-
- Whatever is healthy and works for you
Caregiver guilt – the self-imposed “oughts’,” “shoulds,””shouldn’ts,” and “musts.” Doing or saying what you believe is the wrong thing.
When the guilt and negative emotions rear their ugly heads
When the guilt comes, how about asking yourself what is triggering this? Perhaps an unrealistic belief about your abilities, the unrealistic “oughts,” or faults that are imagined or even unavoidable? You will feel guilty sometimes, don’t try to get rid of it, just accept it. Get comfortable with being uncomfortable. It is hard to accept reality sometimes.
Resentment – few people admit to being or feeling resentment, but it happens quite a lot. It is part of the duality. You love them and want the best for them, but you do feel resentment. Your life got hijacked by this new responsibility. You may be feeling resentment because of feeling slighted by others. Maybe your brothers and sisters do not help? Resentment really shows up when your own life is way out of balance. Yet, another reason to take care of yourself.
Anger – being mad for reasons that are both direct (unfair criticism, a loved one that is not cooperating, too many problems that day) and indirect (you are tired from working full-time, helping your loved one, and the lack of sleep, frustration over the lack of control, disappointment,) Chronic anger and hostility has been linked to high blood pressure, heart attacks, heart disease, stomach problems, headaches and low back pain.
Learn to express your anger in healthy ways when you are a family caregiver
Learn to express your anger in healthy ways. When you blow up or explode, what do you leave in your wake? Who do you hurt? Learn to self-soothe, take a time out, find a constructive way to express your anger. It will take work and practice, but it can be done and you will feel much better and so will your anger targets. Count to five. Take 10 deep breaths. Let your more rational mind catch up to your reactive reptilian mind.
Worry – Worry seems to be good intentions run amok. Our brains need something to focus on or to be engaged with. How many of you are good at ruminating? I know that I can be very good at ruminating. It does nothing but keep me stuck. It is a time waster. It is an energy deplete. It does not change anything. You can “what-if” yourself to death.
Set a timer for 5 minutes and allow worry. When the timer goes off, you then look at the possible solutions to what you have been worrying about. What will be productive? What can make a difference? Who do I need to call?
Loneliness – Caregivers are lonely. Friends step back. Co-workers step back. Some family members step back. You need your peeps. You need them to be present in your life. Go out for lunch or dinner every week or two. Have an afternoon tea and dessert. Take a couple of hours to catch up, laugh, watch a movie, exercise. If you find that your loved ones or friends have stepped back, it may be because they do not want to add to your burdens or they don’t know what to do or how to help you. Be direct and upfront with them. Tell them that you want them to ask you to do things. Tell them that you do want to go out. Tell them to text you or call you and if you can’t talk then that you will contact them later.
Grief – When someone deals with a long-term illness, the grieving process can start soon after diagnosis. Definitely, when the loved one begins to decline. Anticipatory grief is what it is called. I didn’t know it at the time, but that is what happened with me. You are grieving that your loved one is losing their abilities to be the independent person they once were. You are grieving the loss of their abilities that will come.
Defensiveness – It is okay to bristle at some things that people say. Try not to have a knee-jerk reaction to everything that has been said. If you are having a strong reaction to what the other person is saying. Sit with it a minute and figure out why you are feeling defensive. Realize that being overly defensive makes you closed-minded. The kind of person that can’t see the forest for the trees. Most of the time, people are trying to help. Not everyone, but, most are trying to help. The only thing that I will ask you to do is to listen to the suggestion(s) and give them some thought. You get to decide what is best for you and your loved one.
Find support. Find humor where you can. We need to laugh. Even using inappropriate humor is a coping mechanism. Don’t feel guilty about laughing or finding humor in the stressful times. The absurdity of things will make you shake your head. You are not laughing at your loved one. We all know how serious these chronic health conditions are, but we also know there is stupid shit that happens too, and it is funny.
Emotional Acceptance – It has happened, you have an emotional pain.
Try this exercise when you feel safe.
-
- Identify the emotion
-
- Close your eyes and put the emotion 5 feet in front of you (you want to look at it)
-
- Give your emotion a size, shape and color – watch it and recognize it for what it is
-
- Let that emotion return back inside of you
-
- Reflect on what you noticed. Did you notice any change in the emotion when you got some distance from it?
Will you be willing to accept and experience the negative emotion? By accepting the emotion, you are accepting the truth of your situation. You don’t have to expend your energy in trying to deny what is happening. You can focus on solutions. When you accept the emotion, you can be curious about it. Why is it arising? What is it trying to tell you? What tools in your emotional toolbox will help you navigate this emotion and diffuse it? Negative emotions are not fun, and accepting them will not kill you. If you want to lose the destructive power of negative emotions, accept and acknowledge them.
Acceptance is acknowledging the moment as it is, right now. No judgement.
Pat