Stroke, Multiple Sclerosis (MS), Parkinson’s disease, Alzheimer’s disease, Post Traumatic Stress Disorder (PTSD), Traumatic Brain Injury (TBI), Dementia, Epilepsy, Diabetes, & Mental Health disorders
They will need a Care Partner or Caregiver.
What is the difference between a Care Partner and a Caregiver?
Some of you may have never heard the phrase “Care Partner” and are wondering what is the difference between that and a caregiver. A caregiver does things “To” the care receiver and a care partner does things” With” the care receiver. For example, a caregiver may take the spoon and feed the care receiver while the care partner will place their hand under the care receiver’s hand and assists.
Care partners assist with the care while encouraging the person to do all they can do. Yes, it will take longer. Yes, it will probably be messier. Your care receiver needs those successes. They still need to feel useful. They want to contribute, in some way. They want to be as independent as possible and their dignity deserves it.
Are You a Care Partner or a Caregiver?
Quite a few folks never identify as a caregiver or a care partner. They view it as “helping them out.” Taking them to the doctor or to the store is another act of caregiving that is never thought of as caregiving.
Family members, take a look at your role in your care receiver’s life. Is it better for them and you to be a caregiver or a care partner, at this time in your journey? Over time things will change, but right now, what is best? I use both terms interchangeably and am learning that it would be better to use both terms correctly and speak to both the caregiver and the care partner.
I recently saw a new phrase, “Chronic condition care” and I kind of like that, too. We can call it all kinds of things, but we are stuck until the folks providing the help and care identify with those phrases. I look at folks and see that they are clearly Care partners or caregivers, but they never think of themselves that way. Why?
I suppose some think of it as a natural or normal part of the relationship. Some look at it as “just something you do.” Others may fear that if they use the term caregiver, they will have to step up even more and don’t want to do that.
What if you would try the care partnership model first, to improve your loved one’s quality of life? Your role as a care partner may change, over time, but take time to connect with your loved one as you figure out a treatment plan and medication that may help. Strengthen your relationship with your loved one. Communicate what you are feeling (stress and anxiety, fatigue, fear, and whatever else comes up) with your loved one. Too often we clam up and go into protective or preservation mode because of the unknowns. The walls go up and the communication goes way down. Let’s try to reverse this.
If you take on these responsibilities, you are a care partner or caregiver.
If you “help with”, “coordinate care for”, “make appointments for and get them there”, or “see to the care of” …you are a care partner and are probably a caregiver. Yes, even if you don’t do the “hands-on” care. It seems as though the Parkinson’s world has tapped into this Care partner idea much better than the rest of us. Family members and friends can be great Care partners.
Becoming a Care Partner or a Caregiver is a change and sometimes, you don’t want that so you won’t identify with those terms. You are afraid your identity may have to change and you don’t want that. You will help out. What you don’t realize is you are missing out on all of the help available to you and your loved one. It is difficult enough without you making it more difficult.
Being a care partner or a caregiver is hard, but it is not always bad. You don’t have to suffer, hell you can even thrive with the right guidance. Email me and we will set a time to chat and see.
pat@EmpoweringHealthOptions.com
Interesting Read Below:
I saw this on Eurocare and would like to share it with you, The Stages of Caregiving. Read it and see where you are in your journey.
Stage 1: The Expectant Carer
Who are you?
You have a growing concern that, within the near future, your family member or friend will need more and more of your assistance and time. You’re concerned because of your relative’s age, past and present medical condition, and current living condition.
Your keyword: Ask
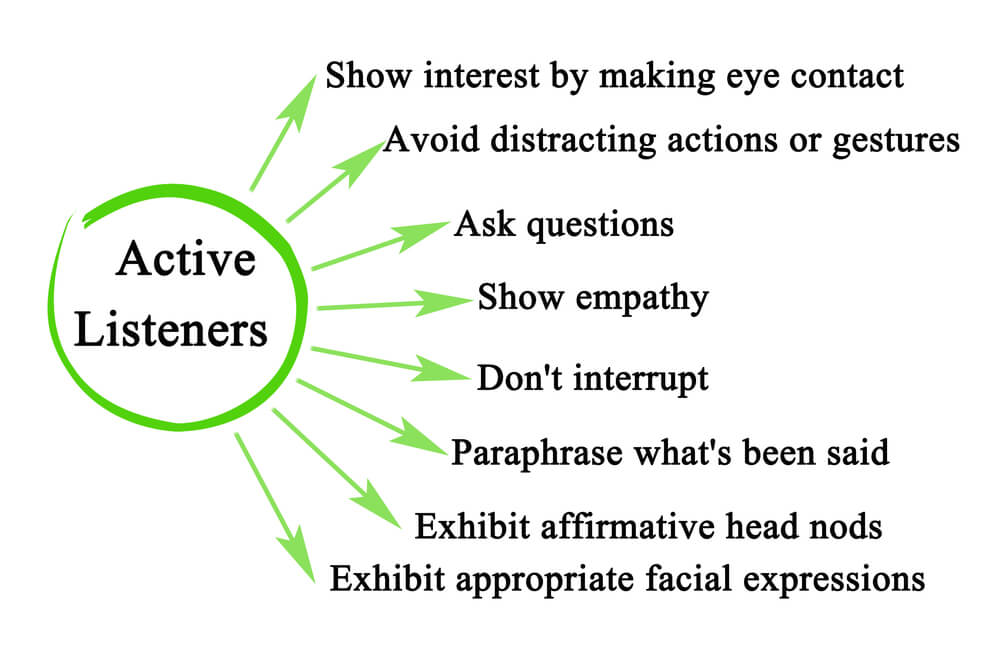
–Ask questions of your caree.
–Ask questions of health care professionals.
–Ask questions of lawyers and financial planners.
–Ask questions of your family members who may be involved in the caregiving role.
Your Challenge
To learn and understand your caree’s needs: health, financial and emotional.
Your Purpose
You expect to become a family carer; this is your time to prepare. You should research options, gather information, and provide the opportunity for your caree to share his or her feelings and values. This is also your time to concentrate on taking care of yourself–keeping up with family and friends, enjoying your hobbies and interests, pursuing your career goals.
As an “expectant carer,” what can you do?
1. Consult with a good lawyer familiar with eldercare issues. Find out about durable powers of attorney for finances and health care as well as living wills; start the process to ensure your caree has the necessary legal papers in order. Ask the attorney: What do we need to know to be prepared for the future? What additional documents will we need? What should we keep in mind? (A durable power of attorney for finances and health care appoints an agent to make decisions on behalf of your caree when he or she is unable to. If you live in one state and your caree in another, consider having documents created for both states)
2. Determine financial situations. Knowing the financial status of your caree can help determine future health care choices. Determine monthly income from pensions and social security; learn about annuities, stock investments and bank accounts. Meet with financial planners to understand how to ensure investments last as long as possible.
3. Investigate community health care options. Which home health care agencies offer quality, affordable home care? Which housing options are available–retirement communities, assisted living centers? Contact community organizations to request brochures and pamphlets. In addition, consider your family member’s current living condition. Will your aging relative be able to reside safely in her home if she uses a wheelchair, becomes bed-bound? What changes can you make today that will prevent future barriers to providing care in her home? Or, are the necessary changes almost an impossibility? If so, what other options do you have: your home, an assisted living facility, a retirement community?
4. Determine the current health care providers. Be familiar with physicians and learn as much as you can about medications.
5. Concentrate on the reality of the situations. Keep a realistic view of your situation: What’s the worst that could happen? What’s the best possible outcome? Then, determine what options are available for each of these outcomes.
6. Start a journal; chronicle your feelings, your concerns and your actions. You may be surprised at feelings of loss. Your preparation of the future allows you to see what your caree–and you–might lose. You both will experience changes in your relationship, your schedules, your amount of freedom. Write down your thoughts about the potential losses–and how you might be able to hang on to them, through minor adjustments and changes, for a little longer.
7. Take time to sort out your own issues. It’s easy to overlook these issues when life seems easy. Caregiving, especially as it intensifies, will make life hard. And, it’s harder if you have unresolved emotional work as it relates to your caree or other family members. If you have difficulty standing up for yourself or finding your voice, this is a good time to work with a therapist or life coach to gain confidence in your decisions and your voice. Do you struggle with the idea of asking for help? Now is a good time to figure out why and start practicing. Knowing how and when to ask for help is a great skill, which will become a huge asset for you. “The Four Agreements, A Practical Guide to Personal Freedom,” a book by Don Miguel Ruiz, offers insights about our personal codes of conduct. As your caregiving journey continues, you’ll interact with family, friends and health care professionals who will drive you nuts. This book will give you the tools so you can stay sane.
8. Find your best shape–physically and financially. Find a work-out routine you like. Maximize the amount of healthy foods you eat. Pay off your debts. Save as much as you can. Uncomfortable managing money? Read books and take classes (online and in your community) to become comfortable. You’ll need to be at your best—physically, emotionally and financially
9. Learn your caree’s life story. Document the story in a journal, video or audio recording. Collect recipes, photos, letters, poems and records that reflect your caree’s life and achievements. Ask questions about your caree’s childhood, parents, siblings and first loves. Involve other family members, including children, in the discussions.
10. Begin each day with the knowledge that you have love. Perhaps the toughest battles in caregiving begin within. Most battles really are about whether or not you are loved—by your caree, by other family members, by friends, by your significant other. End the battle now: Know you have the love. Know it now so you can remind yourself later.
11. An apple a day… What can you do on a regular basis to keep yourself healthy? Be good to yourself—you are too important today (and tomorrow and every day after that) to let your own health slip. In other words, what’s your apple?
Quick Tip: Organize forms and documents that you’ll need in the future.
Stage 2: The Freshman Carer
Who are you?
You’ve begun to help your family member on a regular basis, weekly, perhaps even a few times a week. Your duties range from errand-running and bill-paying to some assistance with hands-on care.
Your keyword: Find
–Find services that help. –Find support that comforts. –Find ways to enjoy your hobbies and interest.
Your Challenge
To discover solutions that work.
Your Purpose
This is your entry into the caregiving role. This is your time to experiment, to get your feet wet and see what works. This is your opportunity to learn how the health care industry works with, or in some cases, against you. Now is the time to shape your caregiving personality: What duties are you comfortable with? What duties make you uncomfortable? How well are you and your caree getting along? What situations would create overwhelming stresses for both of you?
This is also the time when you get a feel for the present and future budgets needed to provide the care your caree requires.
In addition, keep up with your hobbies and interests (you may be able only to keep the ones that you enjoy most), ensuring you have made a habit of spending time on your own, enjoying yourself.
As a “freshman carer,” what can you do?
1. Learn as much as you can about your caree’s illness, disease or condition. Consult the local branches or chapters of national organizations such as The Arthritis Foundation, the Alzheimer’s Association, The Cancer Society. What does the future hold for you and your caree?
2. Learn how to provide proper care from health care professionals or from health care videos, manuals or books. If your caree is hospitalized or receives short-term therapy at a nursing home, ask the staff to show you proper caregiving techniques: lifting, transfers, bathing. Or, search the Internet for hands-on care information.
It’s very difficult to provide care when you are unsure of what you’re doing. You’ll feel much better when you’re confident of your skills.
3. Join a support group–online or in your community. It’s so isolating to be a carer! Support groups will hook you up with others in similar situations; often, you’ll learn of community resources and options from other carers that you were not aware of.
4. Count on regular breaks from caregiving. Plan for regular breaks–an hour daily, an afternoon weekly, or a day monthly–whatever you can manage. Enlist the help of relatives and community services (such as a volunteer group at your local church) so you can take time off regularly. Relatives can help in many ways–through financial support, social support (calling the caree regularly just “to talk”) as well as respite support.
5. Rely on help from community organizations. Meals on Wheels, home care agencies and day care centers, to name just a few, may offer services that your caree needs.
Contact your local Area Agency on Aging for a listing of services and organizations in your community. Visit your local medical equipment supply store to find devices and gadgets that enhance your caree’s abilities–and independence from you. Remember, allowing the help of others is a sign of strength.
In addition, ask about local, state or federal programs that might provide financial assistance for you and/or your caree. As your caree’s care needs increase, so will the costs associated with his or her care. Understanding what programs can help, in addition to understanding what your caree can afford, will help you plan appropriately for the future.
6. Keep your caree’s wishes in mind. If appropriate, ask for his or her input and ideas. Does your caree still feel good about living at home? What does your caree fear or dread? (These are also good questions to ask yourself!)
7. Reflect the changes in your journal. How do you feel now? What are your concerns? Fears? What outcomes are you working toward? What losses have you noticed during this period? What changes in the relationship cause you to feel sad? What changes have given you comfort?
8. Start a second journal that you use to detail your caree’s needs and your caregiving responsibilities. Note any changes in your caree’s health and condition so that you can confidently discuss your concerns during physician appointments. Use your journal as a caregiving manual, which will help when others step in to provide care. Continue to chronicle your caregiving journey in your first journal. What causes you to mourn?
9. Create the habit of regularly holding family meetings. And, if you and your caree share a household with other family members (including children), consider creating House Rules. Rules for the household include:
–Who does what, how and when; –Guidelines for fights, fun, and festivals (celebrations); –Schedule of meetings and their purposes; –Expectations in regard to support, engagement and participation.
10. Manage the money: Develop a budget, keep track of expenses, set up a filing system for bills and receipts. Keep your caree’s expenses separate from yours and your family’s. Keep track (and receipts) of any of your caree’s bills that you pay. If you’re overwhelmed, consider having a professional, like a financial planner or bank trust officer, oversee your caree’s financial situation, including paying bills.
11. Start a Solutions Fund so you can hire solutions. The account funds solutions for boredom, breaks and back-up plans. Contribute a monthly amount; allow yourself flexibility in how you use the monthly budget. Use the fund for your caree, for the house, for you.
Use the Solutions Fund for your caree to hire services such as home health, adult day or to purchase games.
Use the fund for your house (or your caree’s) to hire cleaning service, lawn maintenance, snow removal. The fund buys you services from a counselor or life coach, or for pampering services, adult education classes and activities.
Ask family members to contribute to your Solutions Fund.
12. Have back-up plans and then back-up plans for your back-up plan. Ask yourself, “What if…” and then create a plan to manage the “What if’s.” If it can happen, most likely it will. Be ready with a plan. A geriatric care manager can be invaluable in developing your back-up plans.
13. Build your own paradise of privacy. Call a spare bedroom or a corner in the basement your own. Add your favorite things (books, chocolate, candles, scrapbook, journal, music, TV, videos, photography, family photos) to make the space a retreat you love to use.
14. Continue to maintain your healthy lifestyle. Take note when the stress causes too much comfort food or too few walks. One of your best defenses against the impact of stress is a healthy lifestyle.
15. An apple a day… What’s your apple in this stage? What helps you to feel good on a daily basis? Enjoy your apple every day.
Stage 3: The Entrenched Carer
Who are you?
Your involvement with your caree is almost daily–if not constant. Your caree may live with you–or your involvement means that your day is structured to be available to your caree. You begin to wonder, how much longer can you live this way? Your mood is sometimes upbeat–you’re proud you’ve been able to provide such wonderful care and make decisions that support your caree’s best wishes–and sometimes melancholy–why you? You’ve been mourning the loss of your caree’s abilities and functions and often long for the days before caregiving. And, you’re tired.
Your Keyword: Receive
–Receive help–from anyone who offers; –Receive breaks from caregiving; –Receive support.
Your Challenge
To find the support and strength to continue.
Your Purpose
To develop a routine, create a familiar schedule for both yourself and your caree. A routine will help you deal with the overwhelming stresses and responsibilities that wear you out. A routine will provide comfort for you and your caree–this stage may be the most difficult for both of you. The changes you prepared for in Stage I and II are now a reality–you have become something of a lifeline to a family member or friend.
In addition to your caree’s routine of care, create a routine for yourself. In your routine include: Time for the unexpected; a ritual which begins and ends your day; and a “healthness” activity that nurtures your spiritual, emotional, physical, mental needs.
As an “entrenched carer,” what can you do?
1. Determine your limits in your day and in your role. How long can your caree remain at home? What’s your comfort level in providing care in your home? For instance, some family carers feel uncomfortable providing care when their caree becomes incontinent. Others determine they can provide care at home as long as insurance or Medicare benefits offset some of the home care expenses. Others feel they can provide care as long as their other family members, like spouses and adult children, will put up with it.
Just as important as understanding your limits in your role is recognizing your limits during your day. Consider:
–Which tasks and responsibilities feel like a struggle? –What times during the day do you feel the greatest amount of stress? –When do you find yourself running late, losing your temper, scrambling for a solution? –What do you find yourself dreading or hating? –When do you find yourself in a tug-of-war with your caree? –What times of the day are tough for your caree? –When during the day does your worry about your caree intensify?
When you understand your limits, you can look for help to manage what’s beyond your limits. Understanding your limits will ensure you, your caree and your family will stay in a safe place.
Everyone has limits. What are yours?
2. What are your caree’s limits? Understanding your caree’s limits will help schedule your day and organize your help. Limits will change regularly, so be aware of change in tolerance and fatigue. Not sure how much help to schedule? Add more than you think. You can never have too much.
3. Continue regular breaks. Consider annual weekly breaks–investigate short-term respite stays in your community’s nursing homes. Or, ask relatives to take over the caregiving role for a week or two every year or every two years. Continue to take daily, weekly and monthly breaks. Keep up with your own interests and hobbies as best you can. Take time to enjoy the paradise you built in Stage II.
4. Use your Solutions Fund. Make deposits and take withdrawals, using the money for boredom, breaks and back-up plans.
5. Keep up with a support system–a carer’s support group or empathetic and understand family members or friends.
6. Continue to learn about your caree’s illness or condition. What’s next for your caree? Are you up to the next steps in his or her illness?
7. Increase help as your caree declines. Become comfortable with adding more help as more help is needed. You may think, “I’m okay keeping the level of help as it is.” Unfortunately, keeping the level where your caree was rather than where he or she is will hurt both of you. Note the struggles in the day, then work to add help for you and your caree to manage the struggles.
8. Manage the budget as much as you manage the care. As care needs increase, so does the budget. When you caree has funds to pay for about 18 months in a nursing home, then take note of the situation. This is the time to consider nursing home placement, when your caree’s funds will afford the best choices. Hold a family meeting, tour local facilities, consult with professionals, such as a geriatric care manager. You may decide this isn’t the time to decide. That’s okay. It’s important to be aware that sometimes the budget determines the decision on where a caree continues to receive care.
9. Continue writing in both journals—yours and the other about your caree.
10. Forgive yourself for your bad moments and bad days. They will happen. After they do, give yourself a clean slate to start over.
11. Set boundaries which protect: Your Time; Your Values; Your Well-being, Your Priorities; Your Self. Examples of communicating boundaries include:
–“I’m taking a two-hour break after lunch. I have everything that you’ll need set up in the living room. Thank you so much for helping me enjoy this time. I’m so grateful for your support.” –“I’m uncomfortable with the tone of our discussion. Let’s table our talk until tomorrow.” –“I’m booked, so can’t handle that request. Thank you for thinking of me.”
12. Give you and your caree room for your difficult moments and bad days. When you’re having a tough time, simply say: “I’m having a bad day. I’m taking a few minutes for myself.” When it’s your caree’s turn, say, “I’m sorry you’re having a bad day. I’m going to step away for a few moments.”
13. An apple a day… What’s your apple in this stage? You may feel tempted to sacrifice your apple in this stage. Your apple can’t be sacrificed. Your apple is what makes you feel normal, like yourself. Keep it.
Stage 4: The Pragmatic Carer
Who are you?
You’ve been through it all: hospital admission and discharges; short-term rehab stays in nursing homes; a vast array of community services. You may appear to doubt the advice given by health care professionals; you’ve just been through the health care system long enough to know that sometimes health care professionals may not seem to have your best interest in mind. Some family members and health care professionals worry about your ability to find humor in situations they find offensive. They view your attitude as “calloused” and “uncaring.” Far from it, you have a very practical, very realistic approach toward your caregiving role–and your sense of humor has been a critical tool for your survival. Without your sense of humor, you would have given up a long time ago.
Your Keyword: Welcome
–Welcome the joys of your relationship; –Welcome forgiveness (of yourself, of your caree, of other family members and friends); –Welcome shared activities.
Your Challenge
To gain a greater understanding of yourself and your caree.
Your Purpose
To gain a better understanding of yourself and your caree. You’ve settled into your role and your routine; now is your opportunity to step back and reflect. The first three stages laid the groundwork for this stage, your period of personal growth.
As a “pragmatic carer,” what can you do?
1. Work on finding joy in your relationship with your caree. The biggest joy-killer are your hands-on duties: bathing, dressing, incontinence care. But these duties bring you together, this is your time together. Add some fun to your hands-on care: sing songs, tell jokes, share goals and dreams.
2. Work on forgiving your caree for past hurts. Resentment toward past wrong and injustices will make your present caregiving role very difficult. Let go of what was and concentrate on making what is healthy and productive. Forgiving your caree is one of the best ways you take care of yourself.
3. Develop a habit of enjoying shared activities. Develop a routine of time shared as husband-wife, mother-daughter, father-son rather than as just carer and caree. Releasing the roles of carer and caree allows you to enjoy each other.
4. Begin to think about your future. What goals have you yet to achieve? How can you achieve them? How can your caree help you achieve them?
5. An apple a day… What’s your apple in this stage? What helps you to feel good on a daily basis? You may feel like trying something new. That’s good! You can never have too many apples.
Stage 5: The Transitioning Carer
Who are you?
You’ve been caring for a period of time and now can sense the end.
Your Keyword: Allow
–Allow time to mourn and grieve; –Allow remembrances to remain; –Allow reflections of your experiences.
Your Challenge
To stop the “doing” of caregiving and focus on the “being.” You’re used to doing and going. Now, it’s time to simply be with your caree.
Your Purpose
To walk with your caree during his last months and weeks, implementing his or her decisions about end-of-life care that you both discussed during Stage 1 (or as soon as you could). As you both feel the journey end, this is also a time to mourn and grief. And, this stage is about loving and feeling good about the shared journey. You also will begin to question and worry about the next chapter in your life.
As a “transitioning carer,” what can you do?
1. Use your best judgment as to when you take breaks. You now have a limited amount of time to spend with your caree. Trust your gut and spend as much time as feels right for you. When others encourage you to take a break and you know it’s not the right time, let them know: “Time with my caree is my priority. I appreciate your concern. I’m okay.”
2. Allow yourself time to mourn and grieve. You are experiencing tremendous losses. You’ll feel it.
3. Remember your caree. You don’t have to give away clothes or remove pictures–until you want to. When family and friends seem hesitant to talk about your caree (they worry they will upset you), assure them that sharing memories, laughs and stories brings you great comfort.
4. Reflect back on your caregiving responsibilities and decisions with pride. Find comfort in knowing that you did the best you could.
5. Review your journal. How are you different today than you were on the day you first started writing in your journal? How will you use this experience to enhance your future relationships?
6. An apple a day… What’s your apple in this stage? You may feel that an apple in this stage is unnecessary. Take an apple. It’s what keeps you feeling like you. 7. After Giving. Connect with other former family carers adjusting to a life after caregiving.
Stage 6: The Godspeed Carer
Who are you?
Your role as carer ended more than two years ago. You find yourself compelled to make a difference in the lives of other carers. You share information readily with carers in the earlier stages, you start a business dedicated to helping family carers or you find a job in which you assist family carers. And, you treasure each relationship you have in your life, recognizing that each day, and your health, should never be taken for granted.
Your Keyword: Treasure
–Treasure your dreams; –Treasure your challenges which led to your opportunities and new skills; –Treasure your opportunities to share lessons learned; –Treasure memories of your caree.
Your Challenge
To integrate your former role as a carer into your new life
Your Purpose
To implement your lessons learned from your role as carer, from your caree and from your family members and friends. During this stage, which can last as long you wish, even your lifetime, you reap the benefits of your efforts.
As a “Godspeed Carer,” what can you do?
1. Follow your dreams. Make your goals a reality.
2. Family carers will look to you as a mentor and leader. Allow carers in earlier stages the same freedom to stumble and steady themselves that you had. Share your experiences with expectant carers, freshman carers, entrenched carers and pragmatic carers. They can learn from you!
3. Treasure the memories you have of your caree. Continue to remember your caree regularly through rituals, such as enjoying an ice cream cone in her honor on her birthday, or by planting trees in his honor. Reading and reviewing your diary will be a great way to remember. Of course, your best memorial to your caree’s memory is a life you build for yourself filled with healthy relationships, productive careers and joy and laughter.
4. An apple a day… Your apples kept you going. Now, consider how you’ll use them to create your future. How did your apples change? How did you change? What would you like to try next? Go for it. The world is your apple.
5. After Giving. Connect with other former family carers adjusting to a life after caregiving.
Last Updated on September 9, 2022