November 17, 2021
It would be so much easier if other people just knew what you needed and wanted and did it! No one can read your mind. No one can really understand what you are going through. Even if they have helped take care of a loved one of their own, their needs may have been completely different from your needs. You have to become a more effective communicator. Misunderstandings will occur/ Look, communication is a skill so it can be learned and you can improve communication skills.
Communi-friggin’-cation! It is the key to everything. That is my own word for communication. Did you know that other folks communicate totally different from you, well, maybe it is the understanding that is different? You know what you need, inside of your head, but how do you communicate that need so that others will understand? There are different ways to communicate and people learn differently. Learn to speak in a way that the other person can understand.
Are you one that thinks …
Well, if they knew me…they would know what I need?
I have told them how tired I am and I need a break.
Well, if they could help me, I guess they would.
I talk about how hard it is, all the time. It has taken over my whole life.
No, I’m good, I can just handle it all.
Hey, I need you to be here on Saturday the 8th from 9 am until 6pm.
I need you to do the laundry, change the sheet and provide dinner on Sunday.
How many different styles of communication are there? Four major ones. Body language is another style, but that is for another day. We are talking about being verbal and asking for what you need or want. Wants are okay to ask for too.
Types of Communication Styles
Passive
Passive communicators go with the flow and are sometimes seen as wallflowers. No muss, no fuss. Sometimes they may be unaware of their thoughts or feelings, but more than likely they ignore their own feelings, wants and even their thoughts. They may seem to be easygoing, but underneath anxiety rules. They fear disapproval.
Passive communicators bottle things up. They hardly ever fight and usually cede everything. They stuff and they stuff their feelings and wants. You can stuff things for so long, but they will eventually bubble to the surface. Resentment, here I come!
Aggressive
Aggressive communicators dominate the conversations and state their opinions often overriding others’ opinions. They use direct eye contact, leaning forward, staring at you and moving towards you sometimes. They are very poor listeners and use a harsh tone, even if they don’t mean to be using a harsh tone.
Aggressive communicators are not quiet and yes, they are the ones that yell. They almost never back down. Your feelings will not be considered. Think more of a “win” type personality and not the “win-win” type.
Passive-Aggressive
A passive-aggressive communicator will confuse the hell out of you. Why? Because they cannot get all of their thoughts, and meanings outside of their heads in a cohesive manner or in a way that makes sense to others. They may be easily frustrated. They can become quite irritable and resentful. They will use sarcasm, talk to another person instead of the person that they need to be talking to. They will criticize others. I don’t get this one, but I have seen it happen. They show oppositional behavior. They will be the one that states, “I will help.” They will help and they will Complain the Whole Time. These folks are angry and their words do not match their body language. Gritting their teeth, making their hands into a fist all the while either being indifferent or smiling.
Passive-aggressive communicators are angry and they know that they are angry, but will deny that they are angry or that anything is wrong. Sarcastic barbs coming your way or maybe you will get the silent treatment.
They silently seethe and the other person has no idea what in the world is wrong.
Assertive
An assertive communicator is confident. They are open to discussions and clarifying whatever may be unclear or confusing without being an ass. They are usually calm and will state what they want or need without imposing their requests on others. This type will look for a consensus, if possible. They usually listen and seem to care about others. You may have healthy and loud discussions but it does not feel like you are having an argument. They will share their thoughts, opinions and how they feel about something. They are open to you doing the same. Not only are they able to listen, they are able to hear.
What communication style to you have? What communication style do others in your life have? Can you see how things get all messed up when everyone is talking and no one is listening or hearing?
Improve your communication skills
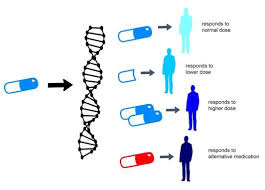
We have all heard it before, seek to understand first. Understand where the other person is coming from, try to put yourself in their shoes. You may not be able to fully, but try as best you can. We all have our own peculiar ways. We are different people with different experiences and we look at things differently. It isn’t wrong, it is just different. Search for common ground. What can you agree on? What is best for the care receiver? What is best for all involved as care givers? Each of us have strengths and each of us have things we don’t do very well. Effective communication decreases stress and helps all of us get on the same page.
Let your empathy and compassion for others help you in moving towards being an assertive communicator. A good sense of humor helps too. Practice active listening and work on communicating clearly.
What strengths help you become a better caregiver?
- Resilience – The ability to withstand or recover quickly from difficult conditions; I can negotiate for what I need and navigate systems.
- Patience – The capacity to accept or tolerate delay, trouble, or suffering without getting angry or upset.
- Flexibility – Ready and able to change so as to adapt to different circumstances; accept what is happening in the moment.
- Compassion – The ability to translate empathic feelings into action (desire to alleviate suffering).
- Optimism – Expect a favorable or positive outcome.
- Confidence – Sure of one’s self and one’s abilities.
- Organization – Methodical and efficient in arrangement or function.
- Ability to Laugh – To easily see and appreciate the humor in the situation.
Use these to rate yourself on the above strengths:
- 1 – Always
-
- 2 – Sometimes
-
- 3 – Hardly ever or Never
Be honest and help yourself to know what you are good at and what you are not so good at… Hopefully, you will find that others have different strengths than you and will be a good helper.
To identify and acknowledge your personal caregiver strengths, set aside a few minutes for personal reflection. Ask yourself the following questions:
- What gives me energy?
- What am I good at? What do I do best? What do I do well?
- What am I naturally good at? What comes naturally to me?
- What are my best character traits?
- What things do I look forward to doing?
- When faced with challenges or adversity, what strengths do I bring to these challenges?
- What do I handle well?
Communicate Effectively
When you ask for things, be specific. Have a list at the ready. You may need things done at your house instead of at the care receiver’s house. Be as flexible as you can. You must agree to a day and time or it will not get done. Never a “whenever” or a “sometime next week.” Pick a day and time, negotiate for another day and time, if necessary. Keep a running list of things that need to be handled. Heck, place it on the refrigerator for folks to sign-up.
Headings for the list include: What action or Task, Where (care receiver’s house or care giver’s house), What day, Alternate day, Who will handle this
You will have to be direct. Not an ass, but state what your Mom/Dad and/or you need their help. Are you willing to step-up, pitch-in and help? If they say yes, then pull out the ready-made list and get to work. If it is a task that takes time and they do not have time, then by all means suggest a less time-consuming task or request a specific amount of money (be fair and reasonable) to hire out the task. If that doesn’t work then ask them what they can contribute and shut your mouth until they begin figuring out things, Yes, it will be uncomfortable, but just be still and quiet. Be open to brainstorming sessions. Try to make your “ask” into statements. For example, instead of saying, “Can you do some things for me?” state that “I need XYZ from the store today.” “I need you to provide dinner on Friday.”
What if you ask and get told “no” to your direct request? You may even get brushed off or told off, where do you go from there? You still need back-up and help. It is going to suck, but you will move forward as if you are an only child. You may need to hire outside help, ideally with the care receiver’s money.
I have seen a family of 4 siblings work it out to care for their aging parents at separate times. They all stepped up and did whatever was needed. They were all professionals and very busy with their careers, but they made their parents the priority. They communicated, worked together, had a list and each of them used their strengths to the fullest. Their parents we never alone.
I have also seen a family with 3 siblings leave it all to one sister. No help, no money, just bitching and “trying” to run things. It was horrible. That one sister realized she would have to handle her mom on her own. She did and her mom was well cared for. It did take some of the sisters’ own money, to help with outside care, but they managed and she had a good experience with her mom for the time her mom had left. She also told me that she had no regrets and that her conscious was clear. She is civil to her siblings, but not really much of a relationship with them now. Of course, it wasn’t much of a relationship before either.
Maybe you will have to say your piece to those that will not contribute in order to let go of your anger or resentment at them. Do let go of your anger, you don’t have the time or energy for it.
There may come a time when you have to say “No” to caregiving.
Communicate your limits
You may find that you must set limits on caregiving responsibilities. You are exhausted, overwhelmed and your own health is suffering. It most often happens to those that do not take care of themselves during the care giving process. You do count. You do matter. Add your needs in to the mix.
What does saying “no” mean to you? Could it mean that you leave the loved one to fend for himself?
Maybe it means that you are tired, isolated and depressed and you have to stop, possibly “no” means that you need to take a breather and you realize that some things will have to change if you are going to proceed and help as a care giver. Boundaries is not a dirty word. Emotional limits are reached quickly when either a crisis happens or you have taken no breaks.
Practice your “I” statements to work on your boundaries.
- “I can no longer drive you to all of your medical appointments due to my work schedule and my limited time off. I know this will be a change for you. I suggest we look into other transportation options such as the Busy Bee Medical Transport Service.”
- “Mother, I am unable to continue with the responsibility of cleaning the house weekly. I want to spend my time with you on other matters. I know it’s hard to let newcomers help, but I think it is time to hire a homemaker service you would be comfortable with.”
- “Dad, I can no longer assist you down the outside stairs. I am worried about your safety and mine. I believe we need to build a ramp for easier access to your home. I have found a carpenter who has reasonable rates for construction.”
In each of the above statements, there is a presentation of what the speaker cannot continue to do, an acknowledgement that the change will have a consequence for the elder and a suggested solution. No attempt is made to make the elder feel guilty about the effort the caregiver is expending or the caregiver’s stress level. It is understood the elder knows the caregiver is working hard.
Setting the boundary is the caregiver’s responsibility. Deborah Colgan, MA, M.Ed., NCC
You can state what you need. You can be direct. You can set boundaries.
Pat