Sleep apnea is a common sleep disorder that affects millions of people worldwide. It is characterized by repeated pauses in breathing during sleep, which can lead to a variety of health issues. One of the most concerning of these is the increased risk of stroke. Studies have shown that people with obstructive sleep apnea (OSA) are up to two to four times more likely to suffer from a stroke than those without the disorder. Despite the clear link between (OSA) and stroke risk, many people are unaware of this connection. In this blog post, we will explore the hidden link between (OSA) and stroke risk, and what you can do to reduce your risk of both conditions. We will also discuss some of the warning signs of sleep apnea and the importance of seeking treatment if you suspect you may have this condition.
1. Introduction: Understanding the prevalence of sleep apnea and stroke
Sleep apnea, a sleep disorder characterized by interrupted breathing during sleep, has become increasingly prevalent in recent years. This condition affects millions of people worldwide, often going undiagnosed and untreated. However, what many may not realize is the potential link between sleep apnea and an increased risk of stroke.
Stroke, a serious medical condition that occurs when blood flow to the brain is disrupted, can have devastating consequences. It can result in long-term disability or even death. While several risk factors for stroke have been identified, such as high blood pressure, smoking, and obesity, the connection between sleep apnea and stroke is still not widely understood.
Research has shown that individuals with (OSA) are more likely to experience cardiovascular issues, including high blood pressure, which is a major risk factor for stroke. During episodes of (OSA), the airway becomes partially or completely blocked, leading to oxygen deprivation. This can trigger a cascade of events in the body, including increased blood pressure and inflammation, which may contribute to the development of stroke.
Furthermore, sleep apnea has been associated with other conditions that are known to increase stroke risk, such as atrial fibrillation and diabetes. These comorbidities, combined with the physiological effects of sleep apnea, create a perfect storm for an increased likelihood of stroke occurrence.
Understanding the prevalence of sleep apnea and its potential link to stroke is crucial for both healthcare professionals and individuals at risk. By raising awareness about this connection, we can promote early detection, appropriate treatment, and lifestyle modifications that may help reduce the risk of stroke.
2. What is obstructive sleep apnea and how does it affect sleep quality?
Obstructive sleep apnea is a common sleep disorder that affects millions of people worldwide. It is characterized by pauses in breathing or shallow breathing during sleep. These pauses, known as apneas, can last for a few seconds to minutes and can occur multiple times throughout the night.
The most common type of sleep apnea is called obstructive sleep apnea (OSA), which occurs when the muscles in the back of the throat fail to keep the airway open. This leads to a blockage in the airflow, causing breathing to temporarily stop. As a result, the brain and body are deprived of oxygen, leading to a disrupted sleep pattern.
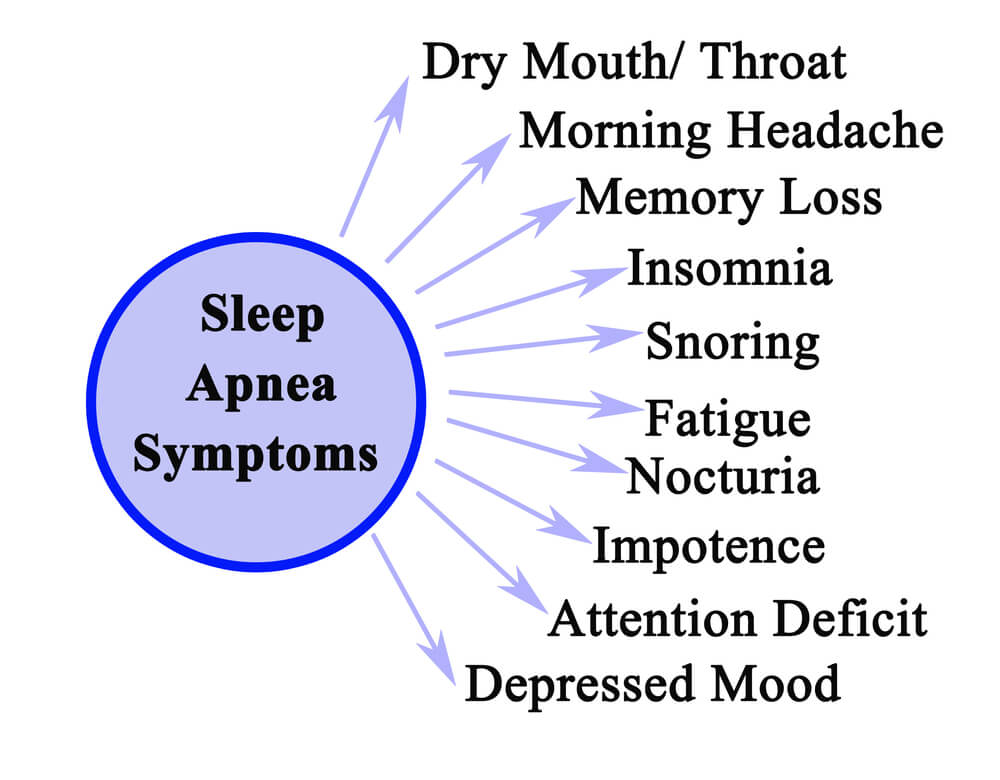
One of the primary symptoms of sleep apnea is loud and chronic snoring, although not everyone who snores has sleep apnea. Other symptoms include excessive daytime sleepiness, morning headaches, difficulty concentrating, and irritability. Sleep apnea can also lead to restless and fragmented sleep, as individuals may wake up gasping for air or choking.
The impact of (OSA) on sleep quality is significant. The constant interruptions in breathing can prevent individuals from achieving deep, restorative sleep. As a result, they may wake up feeling tired and groggy, even after a full night’s sleep. They may have morning headaches. They may also wake up in the middle of the night with a coughing fit. This can have a detrimental effect on overall well-being, as quality sleep is essential for cognitive function, mood regulation, and overall physical health.
Moreover, sleep apnea has been linked to various health complications, including an increased risk of stroke. The intermittent drops in oxygen levels during apneas can trigger a cascade of physiological changes that contribute to vascular damage and inflammation. Over time, this can lead to an increased risk of developing cardiovascular diseases, including stroke.
Understanding the connection between sleep apnea and decreased sleep quality is crucial in recognizing the potential risks associated with this sleep disorder. Recognizing the symptoms and seeking appropriate medical intervention is essential for improving sleep quality, reducing the risk of complications, and promoting overall health and well-being.
3. The link between obstructive sleep apnea and stroke: Analyzing the research findings
One study published in the Journal of the American Medical Association (JAMA) found that individuals with untreated severe sleep apnea were three times more likely to experience a stroke compared to those without sleep apnea. This alarming finding highlights the significant impact that sleep apnea can have on stroke risk.
Further research has revealed that sleep apnea contributes to a variety of factors that can increase the likelihood of stroke. One of the key mechanisms is the intermittent interruption of oxygen supply during episodes of apnea. This oxygen deprivation can lead to the development of various health issues, including high blood pressure, diabetes, and obesity, all of which are known risk factors for stroke.
Additionally, sleep apnea can disrupt the normal sleep patterns and cause excessive daytime sleepiness, impairing cognitive function and increasing the risk of accidents and injuries. These cognitive impairments can further contribute to an increased susceptibility to stroke.
It is worth noting that the relationship between sleep apnea and stroke goes both ways. Not only does sleep apnea increase the risk of stroke, but individuals who have previously experienced a stroke are also more likely to develop sleep apnea. This highlights the importance of addressing sleep apnea as part of stroke prevention and rehabilitation strategies.
While the research findings provide valuable insights into the link between sleep apnea and stroke, further studies are still necessary to fully understand the underlying mechanisms and develop effective interventions. Nonetheless, the existing evidence emphasizes the importance of recognizing and treating sleep apnea as a crucial step in reducing the risk of stroke and improving overall health outcomes.
4. Exploring the mechanisms behind the increased risk factor for stroke in sleep apnea patients
One of the key factors at play is the repeated episodes of oxygen deprivation that occur during sleep apnea. These episodes, known as apneas or hypopneas, lead to a drop in blood oxygen levels, triggering a cascade of physiological responses in the body. This includes an increase in sympathetic nervous system activity and a surge of stress hormones, such as adrenaline and cortisol.
These physiological changes have detrimental effects on the cardiovascular system. Increased sympathetic activity can lead to elevated blood pressure, which is a major risk factor for stroke. The release of stress hormones can also contribute to inflammation and endothelial dysfunction, further promoting the development of atherosclerosis and clot formation.
Furthermore, sleep apnea is often associated with other comorbidities that also contribute to stroke risk, such as obesity, diabetes, and hypertension. These conditions can synergistically interact with sleep apnea, exacerbating the overall risk of stroke.
Another intriguing aspect being explored is the potential impact of sleep apnea on the brain itself. Studies have shown that sleep-disordered breathing, including sleep apnea, may induce structural and functional changes in the brain, particularly in areas involved in regulating blood flow and controlling the autonomic nervous system. These alterations could disrupt the delicate balance of cerebral blood flow and increase the vulnerability of brain tissue to ischemic events
5. The role of oxygen deprivation and sleep disruption in stroke development
During sleep apnea episodes, individuals experience repeated pauses in breathing, leading to a drop in oxygen levels in the body. These episodes can occur multiple times throughout the night, disrupting the normal sleep cycle and causing fragmented sleep patterns. As a result, the brain and other vital organs may not receive an adequate supply of oxygen, leading to a condition known as hypoxia.
The prolonged periods of oxygen deprivation caused by sleep apnea can have detrimental effects on the cardiovascular system. Hypoxia triggers a cascade of physiological responses, including increased blood pressure, inflammation, and oxidative stress. These factors contribute to the development of atherosclerosis, the buildup of plaque in the arteries, increasing the risk of stroke.
Furthermore, sleep disruption caused by sleep apnea can have a significant impact on the body’s stress response. The frequent awakenings and fragmented sleep patterns can lead to elevated levels of stress hormones, such as cortisol. Chronic elevation of these hormones can disrupt the delicate balance within the body, promoting inflammation and further contributing to stroke development.
6. Identifying the risk factors and common symptoms of both sleep apnea and stroke
Identifying the risk factors and common symptoms of both sleep apnea and stroke is crucial in understanding the hidden link between these two conditions. Recognizing these signs can help individuals take proactive steps toward managing their health and potentially reducing their risk of stroke.
Sleep apnea is a sleep disorder characterized by interrupted breathing during sleep. Some common risk factors for sleep apnea include obesity, high blood pressure, smoking, and a family history of the condition. Additionally, age and gender can also contribute to the likelihood of developing sleep apnea, with older individuals and men being at higher risk.
Common symptoms of sleep apnea include loud snoring, gasping or choking during sleep, excessive daytime sleepiness, morning headaches, restless sleep, and difficulty concentrating. It is important to note that not everyone who snores or experiences these symptoms has sleep apnea, but they may serve as warning signs to investigate further.
On the other hand, stroke is a medical emergency that occurs when blood flow to the brain is disrupted, leading to brain cell damage. Certain risk factors for stroke overlap with those of sleep apnea, including obesity, high blood pressure, smoking, and a family history of the condition. Age, gender, race, and certain medical conditions such as diabetes and heart disease also contribute to stroke risk.
Symptoms of a stroke may vary depending on the area of the brain affected but commonly include sudden weakness or numbness on one side of the body, difficulty speaking or understanding speech, severe headache, dizziness, and loss of coordination or balance. Recognizing these symptoms and seeking immediate medical attention is crucial as early intervention can greatly improve the chances of recovery.
7. How to recognize and diagnose sleep apnea to mitigate stroke risk
One of the most common symptoms of sleep apnea is loud and chronic snoring. If you or your partner notice that you snore loudly regularly, it may be an indication of sleep apnea. Other symptoms include frequent awakenings during the night, gasping or choking sensations, morning headaches, excessive daytime sleepiness, and difficulty concentrating.
If you suspect that you or a loved one may have sleep apnea, it is important to consult with a healthcare professional. A sleep study, either conducted in a sleep clinic or through a home sleep testing device, can help diagnose sleep apnea. During a sleep study, various factors such as breathing patterns, brain activity, and oxygen levels will be monitored to determine if sleep apnea is present.
Once diagnosed, treatment options for sleep apnea can help mitigate the risk of stroke. Continuous Positive Airway Pressure (CPAP) therapy is a common treatment method, which involves wearing a mask over the nose or mouth during sleep. The mask delivers a continuous flow of air, helping to keep the airway open and prevent interruptions in breathing.
In addition to CPAP therapy, lifestyle changes can also play a significant role in managing sleep apnea and reducing stroke risk. Losing weight, avoiding alcohol and sedatives before bed, and sleeping on your side can all help improve sleep quality and decrease the severity of sleep apnea.
By recognizing the signs of sleep apnea and seeking proper diagnosis and treatment, individuals can take proactive steps to mitigate the risk of stroke associated with this sleep disorder. Remember, a good night’s sleep is not only essential for overall well-being but also plays a crucial role in maintaining a healthy cardiovascular system.
8. Treating sleep apnea to reduce the risk of stroke: Lifestyle changes, CPAP therapy, and other interventions
When it comes to reducing the risk of stroke, treating sleep apnea can play a crucial role. Sleep apnea is a sleep disorder characterized by pauses in breathing or shallow breaths during sleep. These pauses can last for seconds to minutes and can occur multiple times throughout the night. Not only does sleep apnea affect the quality of sleep, but it has also been found to be closely linked to an increased risk of stroke.
Fortunately, there are various treatment options available to manage sleep apnea and potentially reduce the risk of stroke. Lifestyle changes can be an effective starting point. Weight loss, regular exercise, and avoiding alcohol and sedatives before bedtime can help alleviate symptoms of sleep apnea and improve overall sleep quality.
One of the most common and effective treatments for sleep apnea is Continuous Positive Airway Pressure (CPAP) therapy. This involves wearing a mask over the nose and/or mouth during sleep, which delivers a steady flow of pressurized air to keep the airways open. By ensuring a steady and uninterrupted flow of oxygen, CPAP therapy helps to prevent the pauses in breathing that are characteristic of sleep apnea. By using CPAP therapy consistently, individuals with sleep apnea can experience improved sleep and potentially reduce their risk of stroke.
In addition to lifestyle changes and CPAP therapy, there are other interventions available for treating sleep apnea. This includes oral appliances that help to keep the airway open, positional therapy that encourages sleeping in specific positions to promote better breathing, and in some cases, surgery to correct structural issues that may be contributing to sleep apnea.
It’s important to note that the choice of treatment will depend on the severity of sleep apnea, individual preferences, and recommendations from healthcare professionals. Regular follow-up with a sleep specialist is essential to monitor progress and adjust treatment as needed.
By actively addressing sleep apnea through lifestyle changes, CPAP therapy, and other interventions, individuals can potentially reduce the risk of stroke and improve their overall health and well-being. If you suspect you may have sleep apnea or have been diagnosed with it, it is crucial to seek professional medical advice and explore the appropriate treatment options available to you.
9. The importance of a multidisciplinary approach: Collaboration between sleep specialists and stroke experts
When it comes to understanding the connection between sleep apnea and increased stroke risk, a multidisciplinary approach is crucial. Collaborating between sleep specialists and stroke experts can provide valuable insights and comprehensive care for patients at risk.
Sleep specialists are well-versed in diagnosing and treating sleep apnea, a common sleep disorder characterized by interrupted breathing during sleep. They can conduct sleep studies, analyze the severity of the condition, and recommend appropriate treatments like continuous positive airway pressure (CPAP) therapy or oral appliances.
On the other hand, stroke experts bring their expertise in identifying and managing the risk factors and consequences of stroke. They can assess a patient’s overall cardiovascular health, evaluate any existing stroke risk factors, and provide interventions to reduce the likelihood of a stroke occurrence.
By combining the knowledge and skills of these two disciplines, a more holistic approach can be taken towards patient care. The collaboration between sleep specialists and stroke experts allows for a deeper understanding of how sleep apnea contributes to stroke risk, as well as the development of personalized treatment plans.
Furthermore, this multidisciplinary approach enables healthcare professionals to address other underlying conditions that may be associated with both sleep apnea and stroke, such as hypertension, obesity, and diabetes. By managing these comorbidities effectively, the overall risk of stroke can be further reduced.
In conclusion, the collaboration between sleep specialists and stroke experts is essential in comprehensively addressing the connection between sleep apnea and increased stroke risk. This multidisciplinary approach ensures that patients receive thorough evaluations, personalized treatment plans, and ongoing support to reduce their risk and improve their overall health.
10. Conclusion: Emphasizing the need for awareness, early detection, and effective management of sleep apnea to minimize stroke risk
In conclusion, the link between sleep apnea and an increased risk of stroke is a significant finding that highlights the importance of awareness, early detection, and effective management of this sleep disorder. Individuals, healthcare professionals, and the general public must be educated about the potential consequences of untreated sleep apnea.
By raising awareness about sleep apnea, more people can recognize the symptoms and seek appropriate medical attention. Early detection through regular screenings and diagnostic tests can lead to timely interventions and better outcomes.
Managing sleep apnea effectively is key to minimizing the risk of stroke. Treatment options such as continuous positive airway pressure (CPAP) therapy, oral appliances, and lifestyle modifications can help improve sleep quality and reduce the occurrence of breathing pauses during sleep. Adhering to the recommended treatment plan can significantly reduce the risk of stroke and other associated health complications.
It is also essential for healthcare providers to collaborate with sleep medicine specialists and incorporate sleep apnea screening into routine medical examinations. By working together, they can ensure that patients at risk of sleep apnea are identified and referred for further evaluation and treatment.
In conclusion, recognizing and addressing the relationship between sleep apnea and stroke risk is crucial for safeguarding overall health and well-being. By prioritizing awareness, early detection, and effective management of sleep apnea, we can take significant steps toward reducing the burden of stroke and promoting better sleep health for all.