Managing Chronic Illness: When All You Want to Do is Run Away
People diagnosed with a chronic illness often feel overwhelmed and burdened by their disease and the constant care that comes with it. They may wish to take a break from their illness and enjoy the holidays or simply take a break from the daily routine of managing their condition. However, failing to take care of oneself every day can have serious consequences.
Ignoring the daily care required to manage a chronic illness can lead to a worsening of symptoms, increased medical complications, and a decrease in overall quality of life. It is important for individuals with chronic illnesses to understand the importance of consistent care and to develop healthy habits that allow them to manage their condition without feeling the need to take a break from their disease.
Developing and maintaining healthy habits can be challenging, but individuals with chronic illnesses need to do so. When you have your healthy habits in place, you no longer have to struggle with too many decisions. That is what wears you out. By building a support system, seeking help when needed, and focusing on self-care, individuals can learn to manage their condition and make it a part of their everyday lives. By doing so, they can reduce the impact of their illness on their daily life and improve their overall quality of life.
Key Takeaways
- Consistent care is essential for individuals with chronic illnesses to manage their condition and prevent worsening of symptoms.
- Developing healthy habits and building a support system can help individuals manage their condition and make it a part of their everyday lives.
- Seeking help when needed and focusing on self-care can improve the overall quality of life for individuals with chronic illnesses.
Understanding Chronic Illness
Living with a chronic illness can be challenging and overwhelming. It is important to understand what chronic illness is, the common types and symptoms, and how it impacts daily functioning.
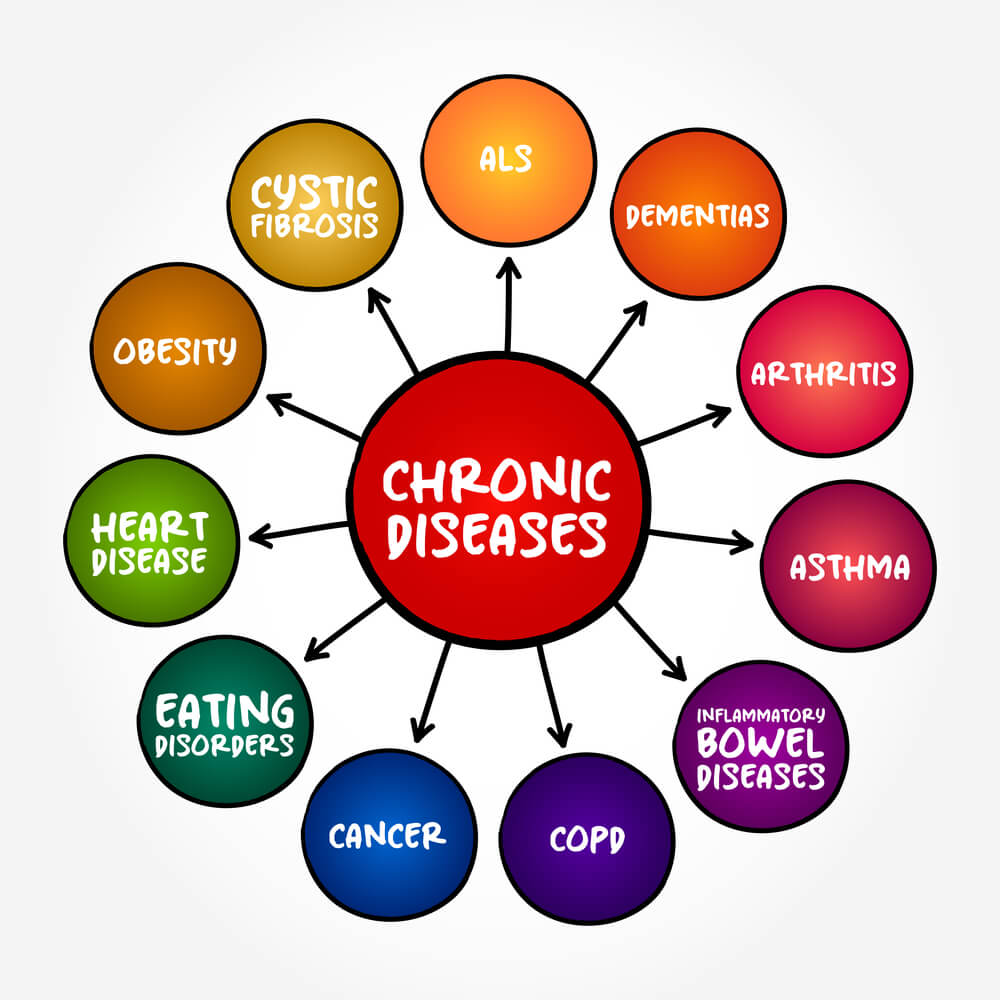
Defining Chronic Diseases
Chronic diseases are long-term conditions that persist for a year or more and require ongoing medical attention. These conditions can affect any part of the body and can range from mild to severe. Chronic illnesses are not contagious and cannot be cured, but they can be managed with proper care and treatment.
Common Types and Symptoms
There are many types of chronic illnesses, including diabetes, arthritis, multiple sclerosis, lupus, chronic fatigue syndrome, cardiovascular disease, cancer, HIV, rheumatoid arthritis, type 2 diabetes, autoimmune diseases, and chronic lung disease (COPD). Each illness has its own unique set of symptoms, but some common symptoms include fatigue, pain, difficulty breathing, and depression.
The Impact on Daily Functioning
Chronic illnesses can have a significant impact on daily functioning, making it difficult to perform everyday tasks and activities. It can also affect a person’s mental health and overall quality of life. However, developing good habits can help manage symptoms and make it easier to cope with the illness. This includes following a healthy diet, exercising regularly, getting enough sleep, and taking medications as prescribed.
In conclusion, understanding chronic illness is an important step in managing it properly. By recognizing the common types and symptoms, individuals can take steps to improve their daily functioning and overall quality of life.
The Psychological Aspect of Chronic Illness
Living with a chronic illness can be emotionally and mentally challenging. People diagnosed with a chronic illness often feel overwhelmed by the physical and emotional demands of the disease. The psychological aspect of chronic illness is an important factor that needs to be addressed in order to manage the condition effectively.
Emotional Consequences
People diagnosed with a chronic illness often experience a range of emotions such as stress, depression, anxiety, fear, guilt, and shame. The emotional consequences of chronic illness can be overwhelming and can impact the person’s quality of life. It is important for individuals with chronic illness to acknowledge and address their emotions in order to manage their condition effectively.
Mental Health and Chronic Illness
Chronic illness can also have a significant impact on mental health. Studies have shown that people with chronic illness are at an increased risk of developing mental health problems such as depression and anxiety. Individuals with chronic illness need to seek professional help if they are experiencing mental health problems.
Developing good habits to deal with chronic illness can make it a part of life that does not feel overwhelming. This can include things like taking medication as prescribed, attending regular check-ups, and adhering to a healthy lifestyle. It is important to establish a support system and to seek help when needed.
Overall, the psychological aspect of chronic illness is an important factor that needs to be addressed to manage the condition effectively. By acknowledging and addressing emotions, seeking professional help when needed, and establishing good habits, individuals with chronic illness can improve their quality of life and manage their condition effectively.
The Importance of Consistent Care
Living with a chronic illness can be overwhelming and challenging, and it can be tempting to take a break from the daily routines of self-care and medical care. However, it is important to understand that consistent care is crucial to managing chronic illnesses effectively.
Medication and Treatment Adherence
One of the essential aspects of consistent care is medication and treatment adherence. Skipping medications or treatments can lead to serious consequences, such as worsening of symptoms, complications, and hospitalization. Therefore, it is crucial to follow the prescribed medication and treatment plan consistently.
Consequences of Neglecting Self-Care
Neglecting self-care can have severe consequences, including fatigue, pain, limitations, and physical functioning. It can also lead to a decline in overall health and well-being. Consistent self-care, such as exercise, healthy eating, and stress management, can help manage symptoms, improve physical functioning, and enhance overall quality of life.
Developing good habits to deal with chronic illness can help make it a part of life, reducing the need to take a break from the disease. It is essential to work with healthcare providers to develop a personalized care plan that suits individual needs and preferences. With consistent care, people living with chronic illnesses can live fulfilling and meaningful lives.
Building and Maintaining Healthy Habits
Living with a chronic illness can be challenging, but building and maintaining healthy habits can make it easier to manage. Establishing a routine and incorporating lifestyle changes can help individuals cope with their illness and prevent the need to take a break from their care.
Establishing a Routine
One of the most important things individuals can do to manage their chronic illness is to establish a routine. This includes taking medications at the same time every day, eating a balanced diet, and getting regular exercise. By establishing a routine, individuals can better manage their symptoms and prevent complications.
Preparing for the day ahead can also help individuals manage their chronic illness. This includes packing medications and snacks, as well as planning for any potential triggers or symptoms. By being prepared, individuals can better cope with their illness and prevent the need to take a break from their care.
Incorporating Lifestyle Changes
In addition to establishing a routine, incorporating lifestyle changes can help individuals manage their chronic illness. This includes making healthy lifestyle choices such as quitting smoking, reducing alcohol consumption, and getting enough sleep.
Having an active coping strategy can also help individuals manage their chronic illness. This includes seeking support from a healthcare provider or support network, setting boundaries, and taking agency over their care. By having an active coping strategy, individuals can better manage their symptoms and prevent the need to take a break from their care.
Overall, building and maintaining healthy habits can help individuals manage their chronic illness and prevent the need to take a break from their care. By establishing a routine, incorporating lifestyle changes, and having an active coping strategy, individuals can better manage their symptoms and live a full and healthy life.
Support Systems and Seeking Help (Especially when you feel overwhelmed.)
When dealing with chronic illness, it is important to have support systems in place. These support systems can come in many forms, including friends, family, healthcare providers, and support groups. Seeking help and support can be crucial in managing the physical and emotional toll of chronic illness.
The Role of Friends and Family
Friends and family can be a great source of support for those living with chronic illness. They can provide emotional support, help with daily tasks, and offer a listening ear. It is important to communicate with loved ones about your needs and limitations, as they may not understand the full extent of your illness.
It is also important to remember that friends and family are not healthcare providers and may not have all the answers. Encourage them to educate themselves about your illness and seek out resources to help them better understand your needs.
Professional Support and Healthcare Providers
Healthcare providers are an essential part of managing chronic illness. They can provide medical care, offer advice on managing symptoms, and help develop a treatment plan. It is important to find a healthcare provider who is knowledgeable about your specific illness and who you feel comfortable talking to.
In addition to medical care, there are also many other forms of professional support available. This can include therapists, social workers, and case managers. These professionals can offer emotional support, help with navigating the healthcare system, and connect you with resources in your community.
Overall, seeking help and support is an important part of managing chronic illness. It is important to build a support system that works for you and to communicate your needs with those around you. With the right support in place, it is possible to develop good habits to deal with your chronic illness and make it a part of your life without feeling the need to take a break from it.
Frequently Asked Questions About Living With A Chronic Illness
What strategies can help in coping with the daily challenges of a chronic illness?
Living with a chronic illness can be challenging, but some strategies can help individuals cope with the daily challenges. Some of these strategies include:
- Developing a routine: Establishing a daily routine can help individuals with chronic illnesses to manage their symptoms and feel more in control of their lives.
- Staying organized: Keeping track of medication schedules, doctor appointments, and symptoms can help individuals with chronic illnesses to stay on top of their care.
- Seeking support: Joining a support group or talking to a mental health professional can help individuals with chronic illnesses to cope with the emotional and psychological challenges of their condition.
How can families support a member dealing with a chronic disease?
Families can play a crucial role in supporting a member dealing with a chronic disease. Here are some ways families can provide support:
- Educating themselves: Learning about the condition and its management can help family members understand what their loved one is going through and how they can best support them.
- Providing emotional support: Offering a listening ear and emotional support can help individuals with chronic illnesses to feel less isolated and more connected to their loved ones.
- Helping with practical tasks: Assisting with tasks such as grocery shopping, meal preparation, and transportation to appointments can help ease the burden on individuals with chronic illnesses.
What are the potential consequences for patients who neglect their chronic illness management?
Neglecting chronic illness management can have serious consequences for patients. Some potential consequences include:
- Worsening symptoms: Neglecting medication schedules, skipping appointments, and ignoring symptoms can lead to a worsening of the condition.
- Increased risk of complications: Neglecting chronic illness management can increase the risk of complications, such as infections or organ damage.
- Reduced quality of life: Neglecting chronic illness management can lead to a reduced quality of life, as symptoms may become more severe and daily activities may become more challenging.
How can individuals with chronic diseases maintain a good quality of life?
Maintaining a good quality of life with a chronic illness can be challenging, but there are steps individuals can take to improve their quality of life. Some of these steps include:
- Staying active: Regular exercise can help improve physical and mental health and reduce the risk of complications.
- Eating a healthy diet: A healthy diet can help individuals with chronic illnesses to manage their symptoms and maintain overall health.
- Engaging in enjoyable activities: Participating in activities that bring joy and fulfillment can help individuals with chronic illnesses to maintain a positive outlook and improve their quality of life.
What are some ways to find acceptance and peace when living with a chronic illness?
Finding acceptance and peace when living with a chronic illness can be a difficult journey, but there are ways to find peace and acceptance. Here are some ways to find acceptance and peace:
- Practicing mindfulness: Mindfulness practices such as meditation and deep breathing can help individuals with chronic illnesses to manage stress and find inner peace.
- Connecting with others: Joining a support group or connecting with others who have similar experiences can help individuals with chronic illnesses to feel less isolated and more understood.
- Focusing on the present: Focusing on the present moment and finding joy in small things can help individuals with chronic illnesses to find acceptance and peace.
How can young adults with chronic diseases effectively manage their health while balancing other life goals?
Managing a chronic illness can be particularly challenging for young adults who are also balancing other life goals such as education, career, and relationships. Here are some ways young adults with chronic diseases can effectively manage their health:
- Prioritizing self-care: Making self-care a priority can help young adults with chronic illnesses to manage their symptoms and maintain overall health.
- Communicating with healthcare providers: Communicating openly and honestly with healthcare providers can help young adults with chronic illnesses to receive the care and support they need.
- Setting realistic goals: Setting realistic goals and breaking them down into smaller, achievable steps can help young adults with chronic illnesses to stay motivated and focused on their health.