Post-stroke depression is a common yet often overlooked condition that affects many stroke survivors. Depression can occur at any point in time after a stroke, but it is more likely to develop during the first year of recovery. It is important to recognize the signs and symptoms of post-stroke depression and seek appropriate treatment to support recovery.
Look, almost everyone is going to be pissed off after having a stroke. That is a normal reaction and so is sadness, anger, and grief. The emotional and physical challenges a stroke survivor faces during recovery and rehab are tremendous. We need to understand that these emotions are more reactional and situational to what is going on in the moment. Post-stroke depression may coexist with anger. It never hurts to have your primary care doctor or your neurologist screen for depression when depressive symptoms occur.
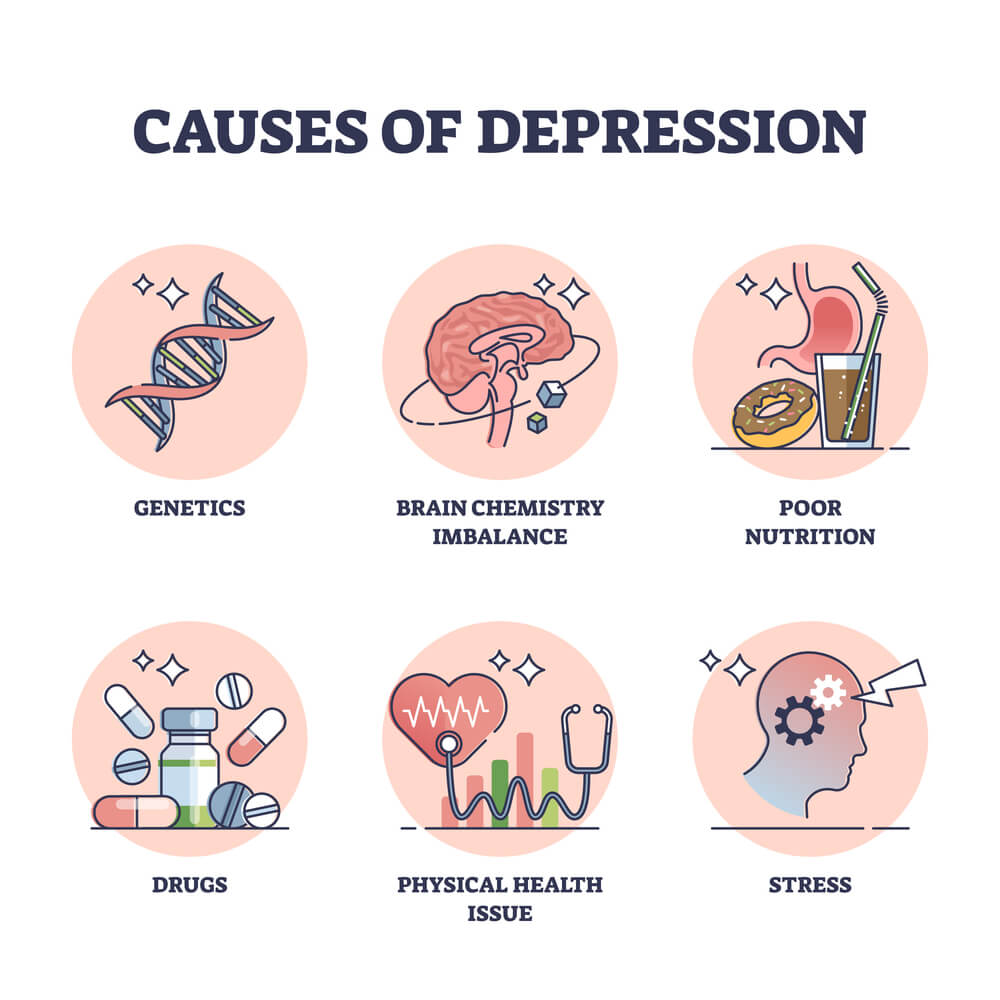
Understanding the risk factors and causes of post-stroke depression is essential in recognizing the signs and symptoms. Some of the common risk factors include a history of depression, severity of the stroke, and social isolation. Symptoms of post-stroke depression can range from persistent sadness and anxiety to feelings of hopelessness and worthlessness. It is important to seek medical attention if any of these symptoms persist for more than two weeks.
Key Takeaways
- Post-stroke depression is a common condition that affects many stroke survivors.
- Recognizing the signs and symptoms of post-stroke depression is essential in seeking appropriate treatment.
- Treatment approaches for post-stroke depression can vary, and it is important to work with a healthcare provider to find the best approach for each case.
Understanding Post-Stroke Depression
Post-stroke depression (PSD) is a common mental health condition that affects stroke survivors. PSD is a type of clinical depression that occurs after a stroke and can significantly impact a person’s quality of life. It is important to understand the signs and symptoms of PSD, as well as the available treatments, to ensure that individuals receive the appropriate care.
Defining Post-Stroke Depression
PSD is defined as a mood disorder that occurs after a stroke. The symptoms of PSD are similar to those of clinical depression and can include feelings of sadness, hopelessness, and worthlessness, as well as loss of interest in once enjoyable activities. Individuals with PSD may also experience changes in appetite and sleep patterns, as well as physical symptoms such as fatigue and pain.
Prevalence and Risk Factors
According to a scientific statement by the American Heart Association, PSD occurs in approximately one-third of stroke survivors at any one time [1]. The exact prevalence of PSD varies depending on the study, but it is clear that PSD is a common condition that affects a significant number of stroke survivors.
Several risk factors have been identified for PSD, including a history of depression, physical disability, and stroke severity [2]. Other risk factors may include social isolation, lack of social support, and cognitive impairment. It is important for healthcare professionals to be aware of these risk factors and to screen stroke survivors for PSD during follow-up visits.
[2] Post-stroke depression: A 2020 updated review
Recognizing the Signs of Post-Stroke Depression
After a stroke, it is common for people to experience a range of emotions. However, if these feelings persist for more than a few weeks and begin to affect daily life, it may be a sign of post-stroke depression.
Post-stroke depression is a common complication that can affect up to one-third of stroke survivors at any time after a stroke. Recognizing the signs and symptoms of post-stroke depression is important so that it can be treated promptly.
Emotional Changes
One of the most common signs of post-stroke depression is a persistent feeling of sadness or hopelessness. People with post-stroke depression may feel tearful, irritable, or anxious for no apparent reason. They may also lose interest in activities they once enjoyed and have difficulty finding pleasure in life.
Behavioral Changes
Post-stroke depression can also cause changes in behavior. People with post-stroke depression may withdraw from social activities and avoid contact with family and friends. They may also experience changes in appetite, sleep patterns, and energy levels.
Cognitive Symptoms of Depression
In addition to emotional and behavioral changes, post-stroke depression can also cause cognitive symptoms. People with post-stroke depression may have difficulty concentrating, making decisions, and remembering things. They may also experience feelings of worthlessness or guilt.
It is important to note that some of these symptoms may be a normal part of the recovery process after a stroke. However, if these symptoms persist for more than a few weeks or begin to affect daily life, it is important to seek help. Treatment for post-stroke depression may include antidepressant medication, talk therapy, or a combination of both.
Current Treatment Approaches
Post-stroke depression (PSD) can be treated effectively using a combination of pharmacological, talk therapy, counseling, and rehabilitation therapies.
Medication Treatments
Pharmacological treatments are a common approach to treating PSD. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are often used to treat PSD. These medications can help alleviate symptoms of depression, such as feelings of sadness, hopelessness, and anxiety. They can also improve sleep and appetite. However, it is important to note that these medications can have side effects, and it may take several weeks or months before their full effects are felt.
Talk therapy and Counseling
Talk therapy can be an effective treatment for PSD. Cognitive-behavioral therapy (CBT) is a common type of psychotherapy used to treat PSD. CBT can help individuals identify negative thoughts and behaviors and replace them with positive ones. Other types of therapy, such as interpersonal therapy (IPT), can also be effective in treating PSD. IPT focuses on improving relationships and communication with others.
Rehabilitation Therapies
Rehabilitation therapies can also be effective in treating PSD. Physical therapy, occupational therapy, and speech therapy can all help individuals recover from stroke and improve their quality of life. These therapies can also help individuals with PSD by providing a sense of purpose and accomplishment. Group therapy and support groups can also help provide social support and reduce feelings of isolation.
It is important to note that treatment for PSD should be tailored to the individual’s needs and preferences. A combination of treatments may be necessary to achieve the best results. It is also important to seek treatment as early as possible to prevent the development of chronic depression and other negative outcomes.
Challenges and Considerations in Treatment
Medication Side Effects
One of the primary challenges in treating post-stroke depression (PSD) is the potential for medication side effects. Antidepressant medications, which are often prescribed to treat PSD, can cause a range of side effects, including nausea, dizziness, dry mouth, and sexual dysfunction. These side effects can be particularly problematic for older adults, who may be more sensitive to the effects of medication.
To address this issue, healthcare providers may need to adjust the dosage or type of medication prescribed to patients with PSD. They may also need to monitor patients closely for side effects and adjust treatment accordingly. In some cases, non-pharmacological treatments such as psychotherapy or cognitive-behavioral therapy may be recommended as an alternative to medication.
Therapy Accessibility
Another challenge in treating PSD is the accessibility of therapy. Many patients with PSD may have physical or cognitive impairments that make it difficult for them to attend therapy sessions or participate in traditional forms of talk therapy. In addition, there may be a shortage of mental health professionals in some areas, making it difficult for patients to access the care they need.
To address these issues, healthcare providers may need to explore alternative forms of therapy that are more accessible to patients with PSD. This could include teletherapy, which allows patients to participate in therapy sessions remotely, or group therapy, which may be more accessible and affordable than individual therapy. In addition, healthcare providers may need to work with community organizations and mental health professionals to increase access to mental health services for patients with PSD.
Supporting Recovery
People who have had a stroke may experience post-stroke depression (PSD), which can make recovery more challenging. Fortunately, there are several ways to support recovery and manage PSD.
Family and Caregiver Support
Family members and caregivers can play a crucial role in supporting a person’s recovery from stroke and managing PSD. They can provide emotional support, help with daily activities, and encourage participation in rehabilitation programs. It is essential for family members and caregivers to understand the signs and symptoms of PSD and to seek help if needed.
Lifestyle Modifications
Lifestyle modifications can also help manage PSD and support recovery. Regular exercise, a healthy diet, and adequate sleep can improve mood and reduce the risk of depression. It is also essential to avoid alcohol and drugs, as they can worsen depression symptoms.
In addition, participating in enjoyable activities, such as hobbies or social events, can improve mood and reduce stress. Meditation and relaxation techniques, such as deep breathing exercises or yoga, can also help manage stress and improve mental health.
Overall, supporting recovery from stroke and managing PSD requires a comprehensive approach that includes emotional support, lifestyle modifications, and professional treatment when needed. By working together, stroke survivors, their families, and healthcare providers can help improve outcomes and quality of life.


