Living with a chronic illness can be a challenging experience that can impact every aspect of a person’s life. Being diagnosed with a chronic illness can be overwhelming, and it can be difficult to know where to turn for support. Patients diagnosed with a chronic illness may wonder how it will affect their daily life, family life, and work life.
Understanding chronic illness is an essential first step in managing it. Chronic illness is a long-term condition that can’t be cured but can be managed. It can affect a person’s physical, emotional, and mental health. Patients diagnosed with a chronic illness may experience a range of emotions, from shock and disbelief to anger, sadness, and fear. Coping with these emotions is an essential part of managing the illness.
Working with healthcare professionals and using complementary alternative medical approaches can help patients manage their chronic illness. Patients should work closely with their healthcare team to develop a treatment plan that meets their individual needs. Complementary alternative medical approaches, such as acupuncture, massage therapy, and meditation, can also help patients manage their symptoms. Having a medical advocate on their side can help patients navigate the healthcare system and ensure that they receive the care they need. Think of Empowering Health Options when you need help.
Understanding Chronic Illness
Living with a chronic illness can be a difficult and life-changing experience. Chronic illnesses are defined as conditions that last for a long period of time and typically cannot be cured. These illnesses can affect nearly every aspect of a person’s life, including their daily routine, family life, and work life.
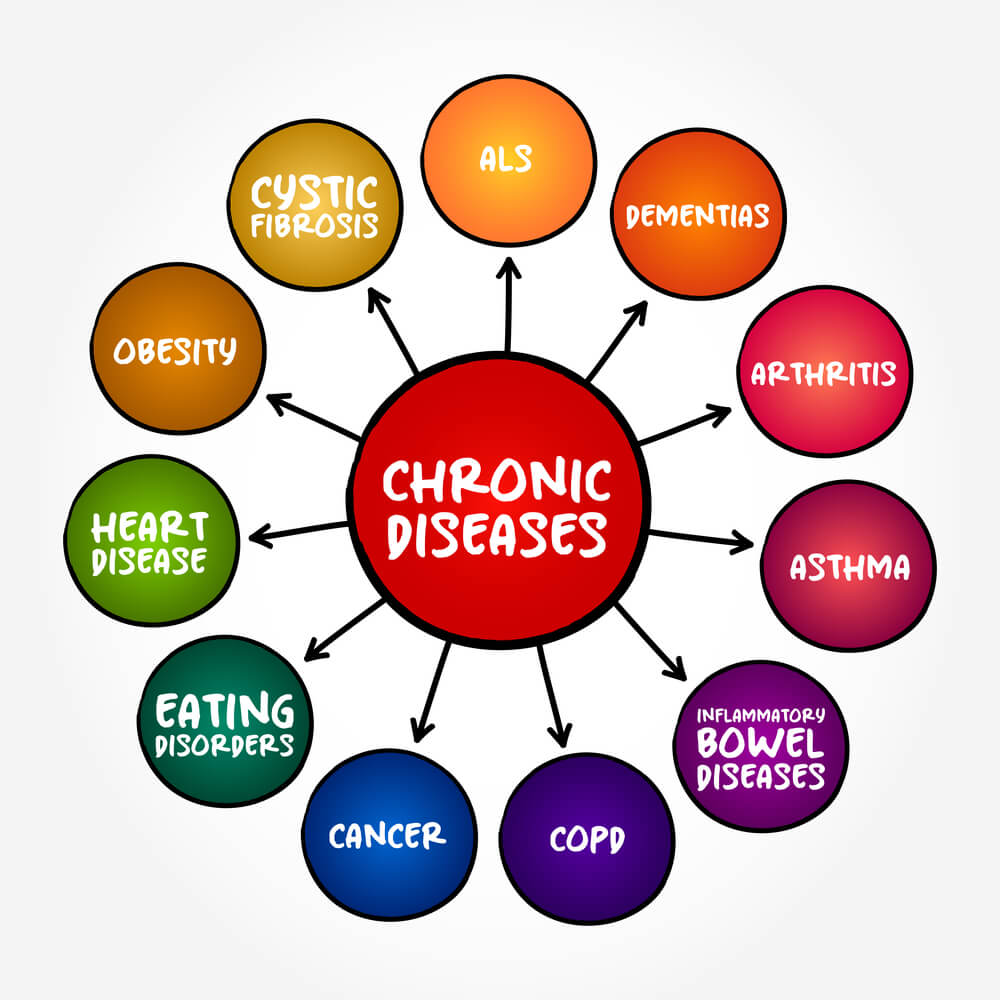
Defining Chronic Disease
Chronic diseases are illnesses that last longer than three months and often develop slowly over time. These diseases can be caused by a variety of factors, including genetics, lifestyle choices, and environmental factors. Some common chronic diseases include diabetes, arthritis, cancer, multiple sclerosis, asthma, heart disease, breast cancer, HIV, stroke, type 2 diabetes, lupus, and rheumatoid arthritis.
Common Chronic Conditions
Diabetes is a chronic disease that affects how the body processes blood sugar. Arthritis is a common chronic condition that causes joint pain and stiffness. Cancer is a group of diseases that involve the uncontrolled growth of abnormal cells in the body. Multiple sclerosis is a chronic disease that affects the central nervous system and can cause a range of symptoms, including fatigue, muscle weakness, and difficulty with coordination. Asthma is a chronic respiratory disease that causes inflammation in the airways, making it difficult to breathe. Heart disease is a chronic condition that affects the heart and blood vessels, and can lead to serious complications such as heart attacks and strokes.
Recognizing the Symptoms
The symptoms of chronic illnesses can vary widely depending on the specific condition. Some common symptoms include fatigue, pain, shortness of breath, swelling, and difficulty with mobility. It is important to recognize the early warning signs of chronic illness and seek medical attention if you experience any unusual symptoms.
Living with a chronic illness can be challenging, but there are many resources available to help patients manage their conditions. Working closely with a physician and using complementary alternative medical approaches can improve a patient’s quality of life. Having a medical advocate on your side can also help navigate the journey of living with a chronic illness.
The Emotional Journey
Being diagnosed with a chronic illness can be a life-altering experience that can trigger a range of emotions. It is normal to feel overwhelmed, anxious, or depressed after receiving a diagnosis. However, it is important to remember that these emotions are a natural part of the grieving process and that it is possible to find ways to cope and move forward.
Initial Reactions to Diagnosis
After receiving a diagnosis, patients may experience a range of emotions, including fear, shock, disbelief, and denial. It is common for patients to feel overwhelmed by the amount of information they need to process, and they may feel uncertain about the future. In some cases, patients may also feel a sense of guilt or shame, wondering if they could have done something to prevent the illness.
Navigating Emotional Challenges
Navigating the emotional challenges of a chronic illness can be difficult, but there are steps patients can take to help manage their emotions. One approach is to seek support from friends, family, or a support group. Connecting with others who have experienced similar challenges can be comforting and can help patients feel less alone.
Another approach is to seek professional help from a mental health provider. Therapy can be an effective way to manage anxiety, depression, and other psychological distress related to a chronic illness. Patients may also find it helpful to practice relaxation techniques, such as deep breathing, meditation, or yoga, to help manage stress and anxiety.
Finding Support
Finding support during the journey of a chronic illness is crucial. Patients may find it helpful to seek out support groups, which can provide a safe and supportive environment for sharing experiences and coping strategies. Support groups can also help patients feel less isolated and can provide a sense of community.
Having a medical advocate can also be beneficial for patients. A medical advocate can help patients navigate the healthcare system, communicate with healthcare providers, and ensure that they receive appropriate care. A medical advocate can also help patients understand their treatment options and make informed decisions about their care.
Impact on Daily Life
Being diagnosed with a chronic illness can have a significant impact on a person’s daily life. Managing symptoms at home, dealing with challenges in the workplace, and navigating relationships and family dynamics can all become more difficult.
Managing Symptoms at Home
Symptoms of chronic illness can vary widely, but common symptoms include fatigue, chronic pain, and changes in physical health. These symptoms can make it difficult to complete daily tasks and can leave people feeling overwhelmed and exhausted.
One way to manage symptoms at home is to establish a routine. This can help people conserve energy and manage their symptoms more effectively. For example, taking breaks throughout the day to rest or meditate can help people feel more energized and focused.
Challenges in the Workplace
Managing a chronic illness while working can be challenging. Fatigue, pain, and other symptoms can make it difficult to concentrate and complete tasks. Additionally, some people may face discrimination or lack of understanding from colleagues or employers.
One way to address these challenges is to work with a physician to develop a plan for managing symptoms at work. This may include making accommodations such as taking breaks or working from home. Additionally, some people may find it helpful to seek support from a medical advocate or disability rights organization.
Relationships and Family Dynamics
Living with a chronic illness can also impact relationships and family dynamics. Partners, families, and elderly relatives may need to provide additional support and care. This can be challenging for everyone involved.
One way to address these challenges is to communicate openly and honestly with loved ones. This can help people understand each other’s needs and work together to provide support. Additionally, seeking support from a therapist or support group can help people navigate these complex relationships.
Treatment and Management
Living with a chronic illness can be challenging, but there are ways to manage and treat the condition to improve one’s quality of life. Treatment and management of chronic illness may involve creating a treatment plan, taking medications, making lifestyle changes, and following a healthy diet.
Creating a Treatment Plan
Creating a treatment plan is an important step in managing a chronic illness. This plan should be developed in collaboration with a physician and should include specific goals and strategies for managing the condition. The plan should also outline how often the patient should see their physician for check-ups and follow-up care.
Medication and Side Effects
Medications are often prescribed to manage chronic illnesses. It is important to take medications as prescribed and to understand the potential side effects. Patients should discuss any concerns they have about medication side effects with their physician. Some side effects may be mild and go away on their own, while others may require a change in medication or dosage.
Lifestyle Changes and Diet
Lifestyle changes and diet can play a significant role in managing chronic illness. For example, physical activity can help improve blood sugar levels and overall health. Patients should discuss with their physician the appropriate level of physical activity for their condition. In addition, following a healthy diet can help manage chronic illness. Patients should work with a registered dietitian to develop a healthy eating plan that meets their individual needs.
Overall, managing a chronic illness requires a comprehensive approach that includes treatment, medication management, lifestyle changes, and diet. Patients should work closely with their physician to develop a personalized treatment plan that meets their individual needs.
Complementary Approaches
When dealing with a chronic illness, patients often turn to complementary alternative medical approaches to improve their quality of life. These approaches can be used in conjunction with traditional medical treatments to help manage symptoms and improve overall well-being.
Alternative Medical Therapies
There are many alternative medical therapies that can be used to complement traditional medical treatments. These therapies include acupuncture, chiropractic care, and herbal medicine. Acupuncture is a form of traditional Chinese medicine that involves the insertion of thin needles into specific points on the body to relieve pain and promote healing. Chiropractic care involves the manipulation of the spine to improve alignment and alleviate pain. Herbal medicine involves the use of plants and plant extracts to treat a variety of health conditions.
It is important to note that while these alternative medical therapies may be helpful, they should not be used as a replacement for traditional medical treatments. Patients should always consult with their physician before trying any new therapies.
The Role of Exercise and Meditation
Exercise and meditation can also be used as complementary approaches to managing chronic illness. Regular exercise can help improve overall health and reduce the risk of developing other health conditions. It can also help manage symptoms of chronic illness, such as fatigue and pain. Meditation can help reduce stress and promote relaxation, which can also help manage symptoms of chronic illness.
Patients should work with their physician to develop an exercise plan that is safe and effective for their specific health condition. Similarly, patients should work with a trained meditation instructor to learn proper techniques and develop a meditation practice that is right for them.
Healing
Finally, it is important to remember that healing is a holistic process that involves the mind, body, and spirit. Patients should focus on taking care of themselves and finding ways to reduce stress and promote relaxation. This can include practicing mindfulness, spending time in nature, or engaging in creative activities.
Having a medical advocate on their side can also be helpful for patients navigating the journey of chronic illness. A medical advocate can help patients understand their medical options, communicate with their healthcare team, and make informed decisions about their health.
By incorporating complementary approaches into their treatment plan and focusing on overall well-being, patients can improve their quality of life and better manage their chronic illness.
Working with Healthcare Professionals
When it comes to managing a chronic illness, building a strong relationship with your healthcare provider is key. This can help you receive the best care possible and ensure that your treatment plan is tailored to your specific needs.
Building a Relationship with Your Doctor
To build a strong relationship with your doctor, it’s important to be open and honest about your symptoms, concerns, and questions. This means being prepared for your appointments by writing down your symptoms, any changes in your condition, and any questions you may have. It’s also important to be honest about any complementary or alternative treatments you may be using, as these can sometimes interact with prescription medications.
Another important aspect of building a strong relationship with your doctor is finding a provider who is a good fit for you. This means looking for a provider who listens to you, takes your concerns seriously, and is willing to work with you to find the best treatment plan for your needs.
The Benefits of a Medical Advocate
Navigating a chronic illness can be overwhelming, which is why having a medical advocate on your side can be incredibly helpful. A medical advocate is someone who can help you navigate the healthcare system, understand your treatment options, and help you become more confident when you talk to your healthcare providers.
A medical advocate can be a family member, friend, or professional advocate. They can attend appointments with you, help you understand medical jargon, and ensure that your needs and concerns are being addressed by your healthcare team.
In addition to providing emotional support, a medical advocate can also help you stay organized by keeping track of your medications, appointments, and treatment plan. This can help ensure that you are receiving the best care possible and can help you feel more in control of your condition.
Overall, working with healthcare professionals and having a medical advocate on your side can help you navigate the challenges of living with a chronic illness. By building a strong relationship with your doctor and finding a supportive advocate, you can improve your quality of life and ensure that you are receiving the best care possible.
Building Resilience and Coping
Living with a chronic illness can be challenging, but there are ways to build resilience and cope with the daily struggles. Here are some tips to help patients navigate this journey:
Developing Coping Strategies
Developing coping strategies is an important part of managing a chronic illness. Coping strategies can help patients deal with stress, anxiety, and depression. Some effective coping strategies include:
- Practicing mindfulness: Mindfulness is a technique that involves focusing on the present moment and accepting it without judgment. Mindfulness can help patients reduce stress and anxiety.
- Staying active: Regular exercise can help patients manage symptoms and improve their overall health. Patients should talk to their doctor before starting any exercise program.
- Setting realistic goals: Patients should set realistic goals for themselves and celebrate their accomplishments. This can help them stay motivated and positive.
- Managing stress: Patients should try to avoid stressors when possible and learn how to manage stress when it is unavoidable. This can include techniques such as deep breathing, meditation, or yoga.
- Seeking support: Patients should seek support from family and friends, or from a therapist or support group. Support can help patients feel less isolated and more connected to others.
Cultivating a Support Network
Cultivating a support network is another important part of managing a chronic illness. Patients should seek support from family and friends, or from a therapist or support group. Support can help patients feel less isolated and more connected to others. Here are some tips for cultivating a support network:
- Communicate openly: Patients should communicate openly with their loved ones about their illness and how it affects them. This can help loved ones understand what the patient is going through and how they can help.
- Build a team: Patients should build a team of healthcare providers, including a primary care physician, specialist, and other healthcare professionals. This team can help the patient manage their illness and coordinate care.
- Join a support group: Support groups can provide patients with a sense of community and understanding. Patients can share their experiences with others who are going through similar challenges.
- Consider a medical advocate: A medical advocate can help patients navigate the healthcare system and advocate for their needs. A medical advocate can also help patients understand their treatment options and make informed decisions about their care.
By developing coping strategies and cultivating a support network, patients can build resilience and manage the challenges of living with a chronic illness.
Long-Term Considerations
Living with a chronic illness means that patients must consider the long-term impact of their condition. Planning for the future is important, and patients should work with their physician to develop a care plan that takes into account the progression of their illness. This care plan should address how the chronic illness will impact their daily life, family life, and work life.
Planning for the Future
Patients with chronic illnesses should plan for the future by considering how their condition may change over time. This may include making adjustments to their living arrangements, such as moving to a more accessible home or seeking assistance from caregivers. Patients should also consider their financial situation and plan for any potential expenses related to their care.
Regular check-ups and tests are important for monitoring the progression of the illness and adjusting the care plan as needed. Patients should also discuss end-of-life care options with their physician and loved ones.
When Illness Becomes Terminal
When a chronic illness becomes terminal, patients and their caregivers must make difficult decisions about end-of-life care. Patients should work with their physician to develop a palliative care plan that focuses on managing symptoms and improving their quality of life.
Caregivers play an important role in providing emotional and physical support during this difficult time. They can help patients navigate the healthcare system and advocate for their needs. Patients may also benefit from the support of a medical advocate who can help them navigate the complex healthcare system and ensure that they receive the best possible care.
Overall, patients with chronic illnesses should focus on maintaining their well-being and quality of life. By working with their physician and exploring complementary alternative medical approaches, patients can improve their daily life and manage their condition effectively.
Frequently Asked Questions
How can chronic illness change my everyday routines and activities?
Chronic illness can have a significant impact on daily life. Depending on the type and severity of the illness, patients may experience physical limitations, fatigue, pain, and other symptoms that can affect their ability to perform routine tasks. For example, someone with arthritis may have difficulty with simple tasks like opening jars or walking up stairs. It is important to communicate with your healthcare provider and loved ones about any changes in your ability to perform daily activities. They can help you find ways to adapt and modify your routine to make things easier.
What are the emotional challenges I might face with a chronic condition, and how can I cope with them?
The emotional impact of chronic illness can be just as challenging as the physical symptoms. Patients may experience feelings of depression, anxiety, frustration, and even grief over the loss of their previous lifestyle. It is important to seek support from loved ones, friends, or a mental health professional to help cope with these emotions. Joining support groups or online communities can also be helpful in connecting with others who are going through similar experiences.
In what ways does a chronic illness affect family dynamics and relationships?
Chronic illness can also have a significant impact on family dynamics and relationships. Family members may need to take on additional responsibilities to help care for the patient, which can create stress and strain on relationships. It is important to communicate openly with loved ones about your needs and to work together to find ways to manage the illness as a team.
How can I maintain a fulfilling work life despite my chronic health issues?
Maintaining a fulfilling work life can be challenging when dealing with chronic illness. Patients may need to make adjustments to their work schedule or responsibilities to accommodate their health needs. It is important to communicate with your employer and coworkers about your needs and to explore accommodations that can help you continue to work. In some cases, it may be necessary to consider a career change or a reduction in work hours to better manage the illness.
What strategies can I use to collaborate effectively with my healthcare provider for better management of my chronic illness?
Effective communication with your healthcare provider is essential for better management of chronic illness. Patients should come prepared to appointments with a list of questions or concerns and be willing to discuss any changes in their symptoms or health status. It is also important to be honest about any complementary or alternative medical approaches being used and to work with the healthcare provider to develop a comprehensive treatment plan.
How can enlisting the help of a medical advocate make a difference in my healthcare journey?
Enlisting the help of a medical advocate can be a valuable asset in navigating the healthcare system and managing chronic illness. A medical advocate can help patients understand their treatment options, communicate with healthcare providers, and navigate insurance and financial issues. They can also provide emotional support and help patients feel empowered in their healthcare journey.


