Pro’s & Con’s of Using Medications to Treat Dementia Behaviors

 Behaviors
Can Behaviors be managed Without Medication? What are the Pro’s & Con’s?
Medications are not without risks. There are no approved medications for behavior management in a dementia. The medications that are being used are being used “off-label.” That means that they are probably being used for a side effect that they cause and not the intended or approved use. Does that make it right or wrong? Each of us has to decide that for ourselves. As long as you understand the risks versus benefits, make the best decision for yourself and know what to look out for as far as other side-effects and adverse reactions. Adverse reactions are things that happen that we do not expect.
In my opinion, it is always better to use non-drug approaches whenever possible. Yes, it will take time and effort, but with consistency behaviors will get better or at least not worsen. Will some eventually need medication? Possibly to Probably. That’s the thing with a chronic illness, there are no absolutes and situations and needs change so be open to the possibility of making other decisions when needed. What is the best decision that you can make, right now, with the information that you have, right now?
Behaviors
Can Behaviors be managed Without Medication? What are the Pro’s & Con’s?
Medications are not without risks. There are no approved medications for behavior management in a dementia. The medications that are being used are being used “off-label.” That means that they are probably being used for a side effect that they cause and not the intended or approved use. Does that make it right or wrong? Each of us has to decide that for ourselves. As long as you understand the risks versus benefits, make the best decision for yourself and know what to look out for as far as other side-effects and adverse reactions. Adverse reactions are things that happen that we do not expect.
In my opinion, it is always better to use non-drug approaches whenever possible. Yes, it will take time and effort, but with consistency behaviors will get better or at least not worsen. Will some eventually need medication? Possibly to Probably. That’s the thing with a chronic illness, there are no absolutes and situations and needs change so be open to the possibility of making other decisions when needed. What is the best decision that you can make, right now, with the information that you have, right now?
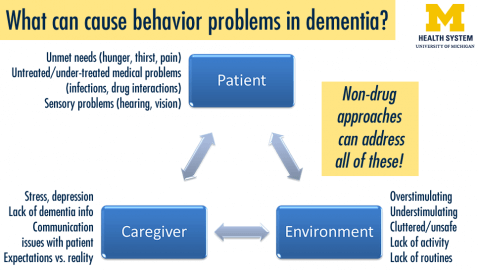
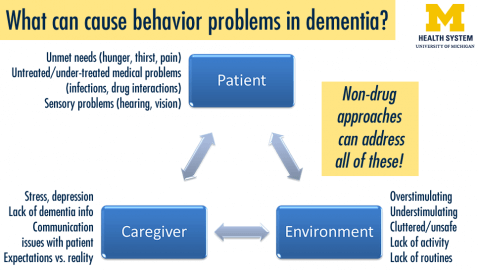
Behaviors have a reason
Drug side effects
Infections
Pain
Discomfort
Uncorrected problems with vision and hearing
How you act and react matters – your attitude and feelings are what they pick up on
You become the detective: Do they have a fever? If yes, call doctor. Do they need to go to the bathroom? Have regular toileting schedule. Are they too hot or too cold in their clothing? Are they bored? Have they had enough exercise during the day? Are they drinking enough?
“DICE” model, Dr. Helen Kales
-
- “D” reminds us to “describe” a disruptive behavior. What is it? When does it occur and with whom? What is the patient perspective on the behavior? How much distress does it cause patient and caregiver?
-
- “I” reminds us to “investigate” the causes of the behavior. Is it an indicator of unrecognized pain, frustration, fear, or boredom? Does it represent medication side effects or an undiscovered medical or psychiatric condition? Is it the result of sensory changes and functional limitations? Does it represent an inappropriate caregiver expectation or a cultural issue?
-
- “C” reminds us to “create” an intervention that addresses the behavior directly. This may include diagnosing and treating pain-inducing physical conditions such as constipation, using a behavioral analysis to craft a behavioral treatment plan, supporting the caregivers, simplifying tasks, finding meaningful activities, or increasing/decreasing stimulation in the environment. Individualized music therapy, for example, can take into account a person’s musical preference and provides soothing music through headphones and an MP3 player. When appropriate, the created intervention may include use of an appropriately chosen and monitored medication.
-
- Finally, the very important “E” reminds us to “evaluate” the effect of the intervention, noting whether it has helped and also whether there have also been unintended consequences or side effects of the intervention.
If nothing physiological is the problem, distract and redirect.
How do you handle issues with other family members wanting to “try” supplement “X, Y or Z?”
As we age, we cannot metabolize and clear medications and supplements as well as we once could and they can and do built up in our bodies. So, the dosage we took in our 50’s may be way too much for us in our 60’s, 70’s and beyond. Supplements can & do cause real harm to people. Don’t be misled by the claims of “Natural,” “Proven,” or even “Improves cognition.” There have been NO large scale, repeatable studies that can prove to the scientific community any supplement or herbal product will help once a person has a dementia. I understand the want, the desire the need for something to help, but that is just not possible at this time. The time to consider using supplements is way before a diagnosis has been made. U.S. National Library of Medicine https://www.nlm.nih.gov/
You can find and research for legitimate studies there with the results of the studies. Let the doctor be the “bad guy” if you need help. Family dynamics, they are usually interesting and quite trying at times. Keep the main thing the main thing, appropriate care and compassion for your loved one. Their bodies cannot metabolize and clear as well as they once did and we are not going to tax the body any more than we have to. Acknowledge their well- meaning ideas and concerns, but state that at this point they need – visits, love, just being with you and sitting or talking. If that doesn’t work then you can just pull out the “Hell to the no!”
Medications
Medications used for depression, anxiety, aggression & restlessness:
Citalopram (Celexa®), Mirtazapine (Remeron®), Sertraline (Zoloft®)
Side Effects
Less common:
-
- Decreased or increased movement
-
- mood or mental changes, including abnormal thinking, agitation, anxiety, confusion, and feelings of not caring
Medications used for severe aggression & restlessness:
Anticonvulsants or Mood Stabilizers – Divalproex sodium (Depakote®), Carbamazepine (Tegretol®), Oxcarbazepine (Trileptal®)
Side Effects
Less common:
-
- bruising burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
-
- change in walking and balance
-
- dizziness, faintness, or lightheadedness when getting up from a lying or sitting position suddenly
-
- lip smacking or puckering
-
- loss of strength or energy
-
- muscle tension or tightness
-
- rapid or worm-like movements of the tongue
-
- seeing, hearing, or feeling things that are not there
-
- shakiness and unsteady walk
-
- unsteadiness, trembling, or other problems with muscle control or coordination
Medications use to treat agitation:
Lorazepam (Ativan®), Clonazepam (Klonopin®), Alprazolam (Xanax ®), Oxazepam (Serax®)
These medications cause sleepiness and possible confusion and an increase risk of falls & dizziness
You want to use the shorter acting ones which are all but the Clonazepam.
Side Effects
Symptoms of overdose:
-
- Changes in patterns and rhythms of speech
-
- loss of strength or energy
-
- shakiness and unsteady walk
-
- unsteadiness, trembling, or other problems with muscle control or coordination
-
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
-
- unusual excitement, nervousness, restlessness, or irritability
-
- unusual paleness unusual weak feeling
Medications used to treat paranoia, hallucinations, severe aggression, and severe agitation:
Antipsychotics – Risperidone (Risperdal®), Quetiapine (Seroquel®), Olanzapine (Zyprexa®)
Less common:
-
- changes in patterns and rhythms of speech
-
- fever, muscle aches, or sore throat
-
- inability to move the eyes
-
- increased blinking or spasms of the eyelid
-
- lip smacking or puckering
-
- rapid or worm-like movements of the tongue
-
- shakiness in the legs, arms, hands, or feet
-
- sores, ulcers, or white spots on the lips or in the mouth
-
- uncontrolled twisting movements of the neck, trunk, arms, or legs
These medications should only be given when the doctor thinks the issues are severe. These have been known to increase mortality in folks with dementia.
Medications used for sleep:
Zolpidem (Ambien®), Ezopiclone (Lunesta®), Zaleplon (Sonata®)
Note – these should only be used if absolutely needed and for only a short amount of time. The person may become more confused and they are at a higher risk of falling.
Side Effects
Less common or rare:
-
- burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
-
- decreased awareness or responsiveness
-
- dizziness, faintness, or lightheadedness when getting up from lying or sitting position
-
- quick to react or overreact emotionally
-
- seeing, hearing, or feeling things that are not there
-
- shakiness in the legs, arms, hands, or feet
Medications that people with AD should not take:
Medications with strong anticholinergic (AC) side effects, such as sedating antihistamines, are well known for causing acute cognitive impairment in people with dementia.
Analgesics – Meperidine (Demerol®)
Antiarrythmics – Disopyramide (Norpace®),
Antidepressants – Amitriptyline (Elavil®), Doxepin (Sinequan®), Imipramine (Tofranil®),
Antiemetics – Promethazine (Phenergan®), Dimenhydrinate (Drammamine®), Meclizine (Antivert®), Cyclizine (Marezine®),
Antipsychotics – Chlorpromazine (Thorazine®), Pimozide (Orap®), Thioridazine (Mellaril®)
Antihistamines – Chlorpheniramine (Chlor-tri-me-ton®), Cyproheptadine (Periactin®), Diphenhydramine (Benadryl®), Hydroxyzine Hcl (Atarax®)
Gastrointestinal & Urinary Antispasmodics – Hyoscyamine (Levsin®), Dicyclomine (Bentyl®), Flavoxate (Urispas®), Oxybutinin (Ditropan®), Tolterodine (Detrol®)
Muscle Relaxants – Carisoprodol (Soma®), Chlorzoxazone (Parafon Forte DSC®), Cyclobenzaprine (Flexeril®), Metaxolone (Skelaxin®), Methocarbamol (Robaxin®), Orphenidrine (Norflex®)
Older adults may be more sensitive to anticholinergic effects in the central nervous system because of age-related changes in pharmacokinetics and pharmacodynamics, reduced acetylcholine mediated transmission in the brain, and increased permeability of the blood-brain barrier. Anticholinergics are known to cause confusion, memory loss, and worsening mental function in people who are older than 65 years.
Acetylcholine is essential for memory and anticholinergics block the release of the neurotransmitter acetylcholine in the central nervous system and the peripheral nervous system.
The way to remember the effects of anticholinergic medications is using the mnemonic Hot as a hare, blind as a bat, dry as a bone, red as a beet, mad as a hatter.
-
- Hot as a hare: increased body temperature
-
- Blind as a bat: mydriasis (dilated pupils)
-
- Dry as a bone: dry mouth, dry eyes, decreased sweat
-
- Red as a beet: flushed face
- Mad as a hatter: delirium
 Behaviors
Can Behaviors be managed Without Medication? What are the Pro’s & Con’s?
Medications are not without risks. There are no approved medications for behavior management in a dementia. The medications that are being used are being used “off-label.” That means that they are probably being used for a side effect that they cause and not the intended or approved use. Does that make it right or wrong? Each of us has to decide that for ourselves. As long as you understand the risks versus benefits, make the best decision for yourself and know what to look out for as far as other side-effects and adverse reactions. Adverse reactions are things that happen that we do not expect.
In my opinion, it is always better to use non-drug approaches whenever possible. Yes, it will take time and effort, but with consistency behaviors will get better or at least not worsen. Will some eventually need medication? Possibly to Probably. That’s the thing with a chronic illness, there are no absolutes and situations and needs change so be open to the possibility of making other decisions when needed. What is the best decision that you can make, right now, with the information that you have, right now?
Behaviors
Can Behaviors be managed Without Medication? What are the Pro’s & Con’s?
Medications are not without risks. There are no approved medications for behavior management in a dementia. The medications that are being used are being used “off-label.” That means that they are probably being used for a side effect that they cause and not the intended or approved use. Does that make it right or wrong? Each of us has to decide that for ourselves. As long as you understand the risks versus benefits, make the best decision for yourself and know what to look out for as far as other side-effects and adverse reactions. Adverse reactions are things that happen that we do not expect.
In my opinion, it is always better to use non-drug approaches whenever possible. Yes, it will take time and effort, but with consistency behaviors will get better or at least not worsen. Will some eventually need medication? Possibly to Probably. That’s the thing with a chronic illness, there are no absolutes and situations and needs change so be open to the possibility of making other decisions when needed. What is the best decision that you can make, right now, with the information that you have, right now?


