We all know someone or someone who has had a stroke. It may or may not be a family member or a friend, but we at least know of someone who is dealing with stroke recovery. Let’s become more aware and understanding of what these folks and their caregivers are dealing with, we must learn more about what a stroke is and how it impacts lives.
Strokes are a leading cause of long-term disability and the fifth leading cause of death in the United States. A stroke occurs when the blood supply to the brain is interrupted, and the brain cells begin to die. This can cause serious damage to the body, including paralysis, difficulty speaking, and memory loss. However, with early detection and proper treatment, it is possible to recover from a stroke. In this post, we’ll take a closer look at the different types of strokes, their causes, and the road to recovery. We will also explore some effective rehabilitation techniques that can help stroke survivors regain their independence and live a full life. If you or a loved one has suffered from a stroke, this post will provide you with valuable information and resources to help rebuild your life after a stroke.
1. What is a stroke?
A stroke is a medical emergency that occurs when blood flow to the brain is interrupted or reduced. It is a sudden and potentially life-threatening event that requires immediate medical attention. When blood flow is disrupted, the brain doesn’t receive the necessary oxygen and nutrients, leading to brain cell damage or death.
There are two main types of strokes: ischemic and hemorrhagic. Ischemic strokes are the most common, accounting for approximately 85% of all stroke cases. They occur when a blood clot or plaque buildup blocks or narrows a blood vessel in the brain. On the other hand, hemorrhagic strokes happen when a blood vessel ruptures, causing bleeding in the brain.
The signs and symptoms of a stroke can vary depending on the area of the brain affected. Common symptoms include sudden weakness or numbness in the face, arm, or leg, especially on one side of the body. Other warning signs may include difficulty speaking or understanding speech, severe headache, dizziness, and loss of balance or coordination.
Recovering from a stroke can be a long and challenging journey. The extent and speed of recovery depend on several factors, such as the severity of the stroke, the area of the brain affected, and the individual’s overall health. Rehabilitation plays a crucial role in helping stroke survivors regain lost skills and improve their quality of life.
Understanding the nature of strokes and their impact is essential for both stroke survivors and their loved ones. By raising awareness and providing information about strokes, we can contribute to a better understanding of this condition and support those on their road to recovery.
2. Understanding the causes and risk factors of strokes
Understanding the causes and risk factors of strokes is crucial in order to prevent and mitigate the impact of this life-altering event. Strokes occur when the blood supply to the brain is disrupted, leading to the deprivation of oxygen and nutrients to brain cells. This disruption can be caused by a blockage in an artery (ischemic stroke) or the rupture of a blood vessel (hemorrhagic stroke).
There are several risk factors that can increase the likelihood of experiencing a stroke. Some of the most common risk factors include high blood pressure, smoking, high cholesterol levels, diabetes, obesity, and a sedentary lifestyle. These factors can contribute to the development of plaque in the arteries, narrowing them and increasing the risk of blood clots that can lead to a stroke.
Other risk factors to be mindful of are age and family history. The risk of stroke increases with age, particularly in individuals over the age of 55. Additionally, if you have a family history of strokes, you may be more susceptible to experiencing one yourself.
It is important to note that while some risk factors cannot be controlled, such as age and family history, many others can be managed and modified through lifestyle changes. By adopting a healthy lifestyle, which includes regular exercise, a balanced diet, quitting smoking, and managing chronic conditions like hypertension and diabetes, individuals can significantly reduce their risk of stroke.
By understanding the causes and risk factors associated with strokes, individuals can take proactive steps to prevent or minimize the impact of this devastating event. Education and awareness are key in empowering individuals to make informed choices and safeguard their health.
3. Recognizing the signs and symptoms of a stroke
Recognizing the signs and symptoms of a stroke is crucial for early intervention and a better chance at recovery. Strokes are often referred to as “brain attacks” and occur when the blood flow to the brain is disrupted, leading to damage to brain cells. It is important to remember the acronym “FAST” when it comes to identifying the warning signs of a stroke.
F – Face drooping: One of the most common signs of a stroke is drooping or numbness in one side of the face. If you notice that someone’s smile appears uneven or one side of their face is drooping, it could be a red flag for a stroke.
A – Arm weakness: Another telltale sign is weakness or numbness in one arm, making it difficult to lift or control. If a person is unable to raise both arms or experiences sudden weakness in one arm, it could indicate a stroke.
S – Speech difficulties: Slurred speech or difficulty speaking and understanding others is another symptom to watch out for. If someone’s speech is suddenly impaired or they are having trouble finding the right words, it may be a sign of a stroke.
T – Time to call emergency services: Time is of the essence when it comes to treating a stroke. If you observe any of the above symptoms, it is vital to call emergency services immediately. Quick medical attention can significantly reduce the potential damage caused by a stroke and improve the chances of a successful recovery.
It is important to note that strokes can also present with other symptoms such as sudden severe headaches, dizziness, trouble walking, and vision problems. While these may not be as common, they should not be ignored.
Being able to recognize the signs and symptoms of a stroke is crucial not only for the affected individual but also for their loved ones and those around them. By staying informed and spreading awareness about strokes, we can help save lives and improve the outcomes of those who experience these life-altering events.
4. The impact of strokes on individuals and their families
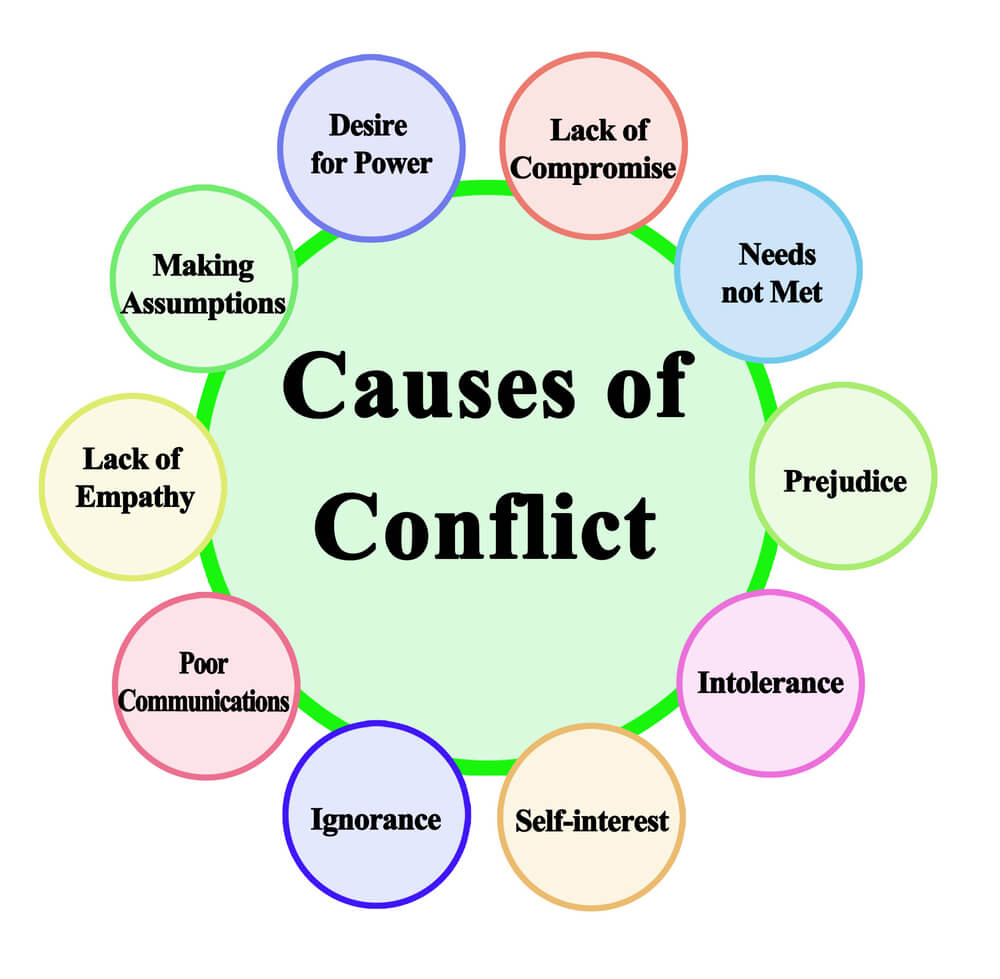
Strokes can have a profound impact on individuals and their families, often turning their lives upside down in an instant. The physical and emotional toll of a stroke can be devastating, leaving individuals struggling to perform even the simplest tasks they once took for granted.
Physically, strokes can cause paralysis or weakness in one side of the body, making it difficult for individuals to perform basic functions such as walking or dressing themselves. Everyday activities like cooking, cleaning, and going to work may suddenly become insurmountable challenges.
But the impact of strokes goes beyond physical limitations. They can also affect cognitive abilities, including memory, speech, and problem-solving skills. This can lead to frustration and a loss of independence, as individuals struggle to communicate or remember important details.
The emotional toll of strokes cannot be underestimated either. Individuals may experience feelings of grief, anger, or depression as they come to terms with the sudden changes in their lives. For families, witnessing their loved one’s struggle can be incredibly difficult, as they navigate the role of caregiver and adjust to the new normal.
However, it is important to remember that strokes do not define a person’s identity or potential for recovery. With the right support and rehabilitation, individuals can make remarkable progress in rebuilding their lives. Physical therapy, occupational therapy, and speech therapy can all play a crucial role in helping stroke survivors regain independence and improve their quality of life.
Additionally, support groups and counseling can provide individuals and their families with the emotional support they need to navigate the challenges of stroke recovery. Connecting with others who have gone through similar experiences can be incredibly empowering, offering a sense of community and understanding.
Understanding the impact of strokes on individuals and their families is essential in providing the necessary support and resources for recovery. By raising awareness and promoting education about strokes, we can help create a more compassionate and inclusive society for stroke survivors and their loved ones.
5. The road to recovery: Understanding the stroke rehabilitation process
The journey to recovery after a stroke can be both challenging and rewarding. Understanding the rehabilitation process is crucial in providing the best care and support for stroke survivors. Rehabilitation aims to help individuals regain lost abilities, improve their overall functioning, and regain independence.
The rehabilitation process typically begins as soon as possible after a stroke, often starting while the individual is still in the hospital. It involves a multidisciplinary team of healthcare professionals, including physiotherapists, occupational therapists, speech-language pathologists, and psychologists, working together to address the specific needs of each patient.
Physiotherapy plays a central role in stroke rehabilitation, focusing on improving mobility, strength, and balance. Through targeted exercises and techniques, physiotherapists help stroke survivors regain control over their movements and enhance their overall physical abilities. This may include exercises to improve walking, stretching to increase flexibility, and strength training to rebuild weakened muscles.
Occupational therapy focuses on helping individuals regain independence in performing daily activities. This may involve relearning skills such as dressing, bathing, eating, and using the bathroom. Occupational therapists also assess the home environment and recommend modifications or assistive devices to facilitate a safe and accessible living space.
Speech-language therapy is vital for stroke survivors who may experience difficulties with speech, language, and swallowing. Speech-language pathologists work on improving communication skills, addressing speech impairments, and providing strategies for effective communication. They also help individuals overcome swallowing difficulties through specialized therapy techniques.
Psychological support is an integral part of stroke rehabilitation. Dealing with the physical and emotional impact of a stroke can be overwhelming for both the survivor and their loved ones. Psychologists and counselors provide individual and group therapy to address emotional challenges, coping strategies, and adjustment to life after a stroke. They also offer support for managing stress, depression, and anxiety that may arise during the recovery process.
It is important to note that stroke recovery is a unique journey for each individual, and the duration and outcome of rehabilitation can vary. The road to recovery requires patience, perseverance, and a supportive network of healthcare professionals, family, and friends. With proper rehabilitation interventions and ongoing support, stroke survivors can regain independence, improve their quality of life, and rebuild their lives after stroke.
6. Rehabilitation therapies and techniques for stroke survivors
Rehabilitation plays a crucial role in the recovery journey of stroke survivors. After experiencing a stroke, individuals often face various physical, cognitive, and emotional challenges that can significantly impact their daily lives. Rehabilitation therapies and techniques are designed to address these challenges and help stroke survivors regain independence and functionality.
Physical therapy is a fundamental component of stroke rehabilitation. It focuses on improving mobility, strength, and coordination. Through targeted exercises and activities, physical therapists work with stroke survivors to restore their ability to walk, perform daily tasks, and engage in physical activities. These sessions may include gait training, balance exercises, and muscle strengthening routines tailored to the individual’s specific needs.
Occupational therapy is another vital aspect of stroke rehabilitation. This therapy aims to assist stroke survivors in relearning essential skills for daily living, such as dressing, eating, and bathing. Occupational therapists provide guidance and utilize adaptive techniques or assistive devices to help stroke survivors regain independence in performing these activities. They may also focus on cognitive rehabilitation to enhance memory, problem-solving, and decision-making abilities.
Speech and language therapy is often necessary for stroke survivors who experience communication difficulties, such as aphasia. Speech therapists work with individuals to improve speech clarity, language comprehension, and expression. They may also provide alternative communication methods, such as using gestures or augmentative and alternative communication (AAC) devices, to facilitate effective communication.
In addition to these core therapies, stroke rehabilitation may involve other specialized approaches. For instance, constraint-induced movement therapy restricts the use of the unaffected limb to encourage the affected limb’s use and regain motor function. Virtual reality-based therapies offer an immersive and engaging environment for stroke survivors to practice movements and improve motor skills. Cognitive-behavioral therapy may be beneficial for addressing emotional and psychological challenges that often accompany stroke recovery.
It is important to note that stroke rehabilitation is highly individualized, as each stroke survivor’s needs and goals are unique. Therefore, a comprehensive evaluation by a multidisciplinary team of healthcare professionals is essential for designing a personalized rehabilitation plan. By combining various therapeutic techniques, stroke survivors can make significant progress on their road to recovery and rebuild their lives with confidence and determination.
7. Assistive devices and technologies for stroke recovery
Assistive devices and technologies play a crucial role in the journey of stroke recovery. These innovative tools offer a lifeline to individuals affected by strokes, helping them regain independence and improve their quality of life.
One such device is the robotic exoskeleton, which assists stroke survivors in regaining mobility and retraining their muscles. These exoskeletons provide support and guidance during physical therapy sessions, helping patients relearn movements and rebuild strength. By utilizing sensors and actuators, these devices mimic natural human motion, aiding in the rehabilitation process.
Another important assistive technology is the use of brain-computer interfaces (BCIs). BCIs enable individuals with limited mobility to control electronic devices using their brain signals. This technology not only empowers stroke survivors to communicate effectively but also facilitates the performance of daily tasks such as operating a wheelchair or turning on lights. By bypassing the need for physical movements, BCIs offer newfound independence and autonomy.
In addition to these advanced technologies, there are a plethora of assistive devices available to aid in stroke recovery. These range from simple tools like reachers and grab bars to more complex devices like adaptive keyboards and voice-activated assistants. These assistive devices are designed to compensate for physical impairments, making daily activities more manageable and promoting self-sufficiency.
It is important to note that assistive devices and technologies should be tailored to each individual’s specific needs. Working with healthcare professionals and rehabilitation specialists is crucial in determining the most suitable devices for stroke survivors. Additionally, ongoing support and training are essential to ensure proper usage and maximize the benefits of these assistive technologies.
By embracing these assistive devices and technologies, stroke survivors can navigate the road to recovery with increased confidence and independence. These innovations not only provide practical assistance but also instill hope and inspire individuals to rebuild their lives after stroke.
8. Emotional and psychological support for stroke survivors
Emotional and psychological support plays a crucial role in the recovery journey of stroke survivors. Dealing with the aftermath of a stroke can be overwhelming, both for the survivors and their loved ones. It is not just the physical challenges that they face, but also the emotional and psychological impact that can greatly affect their well-being.
Stroke survivors may experience a wide range of emotions such as frustration, sadness, anger, anxiety, and even depression. The sudden change in their abilities and independence can be difficult to accept. It is essential to provide a supportive environment that acknowledges and validates these emotions.
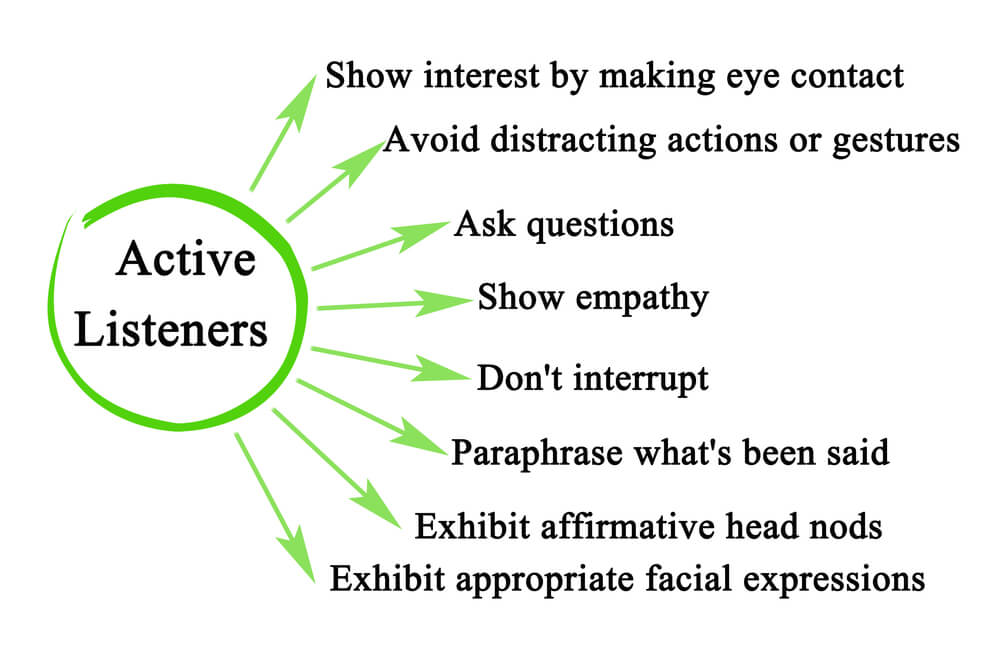
One effective way to offer emotional support is through counseling or therapy sessions. These sessions can help survivors and their families navigate through the complex emotions and challenges that arise post-stroke. Professional therapists can provide a safe space for individuals to express their feelings, address any psychological issues, and develop coping strategies.
Support groups specifically tailored for stroke survivors can also be incredibly beneficial. Connecting with others who have gone through similar experiences can create a sense of community, understanding, and shared knowledge. These support groups allow individuals to share their stories, exchange advice, and provide mutual encouragement, fostering a sense of belonging and empowerment.
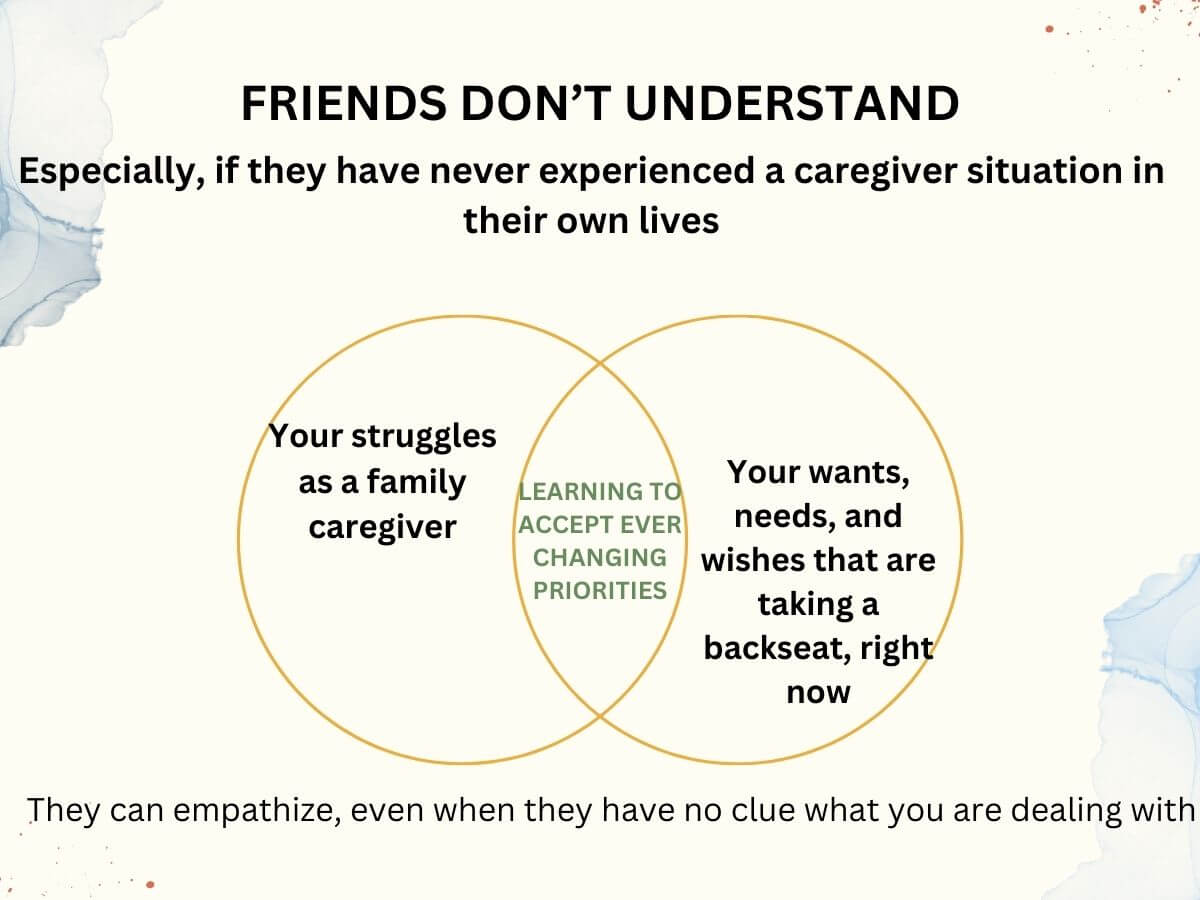
Additionally, caregivers and family members of stroke survivors also require emotional support. The role of a caregiver can be demanding and emotionally draining. Providing resources and outlets for them to seek support, such as support groups or counseling, is vital to prevent caregiver burnout and ensure the overall well-being of everyone involved.
It is important to recognize that the emotional and psychological recovery from a stroke is a journey that takes time and patience. Offering ongoing support and understanding can make a significant impact on the overall quality of life for stroke survivors, helping them rebuild their lives and regain a sense of normalcy.
9. Tips for caregivers and loved ones of stroke survivors
Taking care of a stroke survivor can be a challenging and emotionally demanding task. As a caregiver or loved one, your support and understanding are crucial in helping the stroke survivor navigate their road to recovery. Here are some essential tips to assist you in this important role.
1. Educate Yourself: Take the time to learn about strokes, their effects, and the recovery process. Understanding the physical, emotional, and cognitive challenges faced by stroke survivors will enable you to provide better care and support.
2. Patience and Empathy: Recovery from a stroke can be a slow and frustrating process. Be patient with the survivor and offer empathy during their moments of struggle. Encourage them to stay positive and remind them of their progress, no matter how small.
3. Encourage Independence: While it is important to provide support, it is equally crucial to encourage independence. Help the stroke survivor regain their confidence by allowing them to perform tasks they are capable of doing. This will boost their self-esteem and aid in their overall recovery.
4. Create a Supportive Environment: Make modifications to the living space to ensure it is safe, accessible, and conducive to recovery. Remove any tripping hazards, install grab bars in the bathroom, and arrange furniture for easy navigation. Additionally, provide emotional support by creating a positive and nurturing atmosphere.
5. Establish a Routine: Establishing a structured daily routine can provide stability and a sense of control for the stroke survivor. Create a schedule for therapy sessions, medication, meals, and rest, and stick to it as much as possible. Having a routine helps the survivor regain a sense of normalcy and aids in their rehabilitation.
6. Take Care of Yourself: As a caregiver or loved one, it is essential to prioritize self-care. Make sure to attend to your physical and emotional well-being. Seek support from friends, family, or support groups to prevent burnout and maintain your ability to provide care effectively.
7. Seek Professional Help: Don’t hesitate to seek professional assistance when needed. Consult with healthcare professionals, therapists, or support groups to gain further insights and guidance. They can offer valuable resources, advice, and coping strategies for both the survivor and the caregiver.
Remember, your role as a caregiver or loved one is crucial in the stroke survivor’s recovery journey. Your support, understanding, and dedication can make a significant difference in rebuilding their lives after a stroke.
10. Inspiring stories of stroke survivors and their journey to rebuilding their lives
The journey to rebuilding one’s life after a stroke is undeniably challenging, both physically and emotionally. However, it is often through these stories of resilience and determination that we find inspiration and hope. In this section, we will delve into the inspiring stories of stroke survivors who have defied the odds and embarked on a transformative journey of rebuilding their lives.
Meet Sarah, a vibrant and successful businesswoman who, at the peak of her career, was struck by a stroke that left her paralyzed on one side of her body. With unwavering determination, Sarah refused to let this setback define her. Through months of intensive rehabilitation, countless hours of physical therapy, and the unwavering support of her loved ones, Sarah gradually regained her strength and mobility. Today, she not only walks confidently but has also returned to her professional life, inspiring others with her resilience and unwavering spirit.
Then there is Mark, an avid adventurer whose world came crashing down when a stroke left him with speech and memory difficulties. Undeterred, Mark embarked on a challenging journey of relearning communication skills, embracing cognitive therapies, and pushing his limits. Through sheer determination and the support of his rehabilitation team, Mark not only regained his ability to communicate but also embarked on new adventures, proving that a stroke does not have to be the end of one’s dreams.
These stories of stroke survivors highlight the incredible strength and resilience that lie within each individual. They serve as a reminder that with the right support, determination, and rehabilitation, one can overcome the physical and emotional challenges brought on by a stroke.
If you or a loved one are currently on the road to recovery after a stroke, take solace in these inspiring stories. Remember that you are not alone in your journey, and with time and perseverance, you too can rebuild your life and embrace a new sense of purpose and hope.