You feel the tightening in your upper traps and neck. You feel yourself breathing harder and shallower and probably the teeth clenching has begun. Something or someone has just impeded your progress or disrupted your flow.
Stress is unavoidable but it does not have to knock you for a loop every time. Something or someone is always going to throw a monkey wrench in your plans. You can stop being surprised. Start expecting it. Yes, indeed…expect it. Why? So you can figure out a workaround or at the very least you can learn to take a breath or three and calm your ass down BEFORE you do or say something that you will probably regret.
It is your response that is causing you pain.
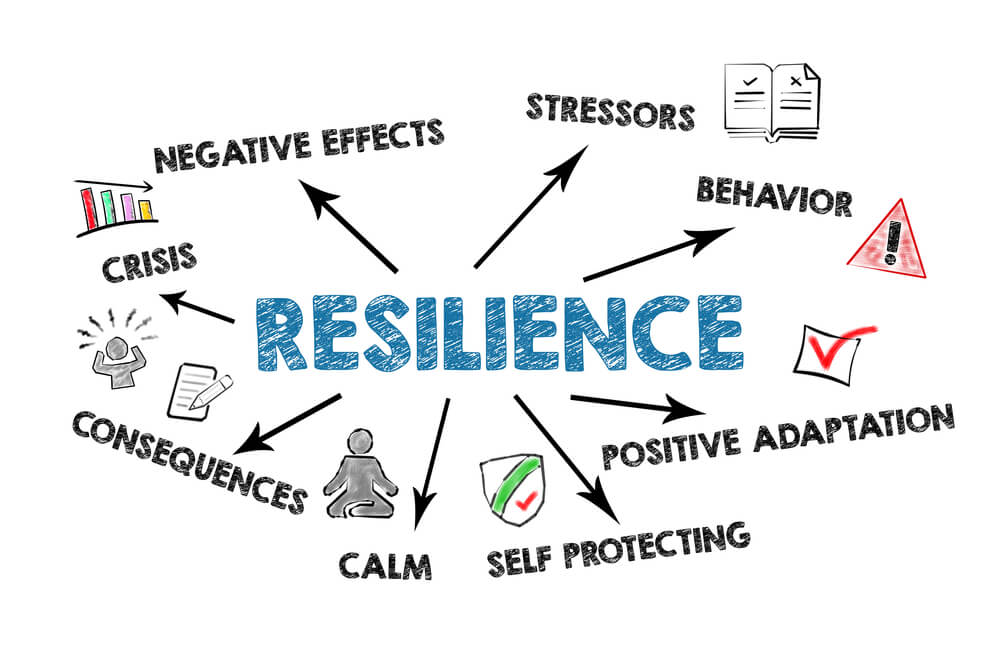
Many people experience stress in their daily lives. Stress can be caused by a variety of factors such as work, relationships, and financial issues. It is important to identify the sources of stress in your life and learn how to manage them effectively. Building resilience can help you cope with stress and bounce back from difficult situations.
Identifying stress in your life can be challenging, but it is an important first step in managing it. Common signs of stress include irritability, fatigue, difficulty sleeping, and changes in appetite. Stress can also cause physical symptoms such as headaches, muscle tension, and stomach problems. By paying attention to these signs, you can begin to identify the sources of stress in your life and take steps to manage them.
Building resilience is another key strategy for managing stress. Resilience is the ability to adapt to difficult situations and recover from adversity. It involves developing coping skills, building social support networks, and maintaining a positive outlook. By building resilience, you can better manage stress and improve your overall well-being.
Understanding Stress
Stress is a natural response to a challenging situation. It can be beneficial in small doses, but when it becomes chronic, it can harm one’s health and well-being. In this section, we will explore the signs and symptoms of stress and the common causes of stress.
Signs and Symptoms of Stress
Stress can manifest in many ways, both physically and emotionally. Some common signs and symptoms of stress include:
- Headaches
- Muscle tension or pain
- Fatigue
- Difficulty sleeping
- Irritability or anger
- Anxiety or depression
- Changes in appetite
- Difficulty concentrating
It’s important to note that everyone experiences stress differently, and what may be stressful for one person may not be for another. However, if you notice any of these symptoms in yourself or a loved one, it may be a sign that stress is becoming a problem.
Common Causes of Stress
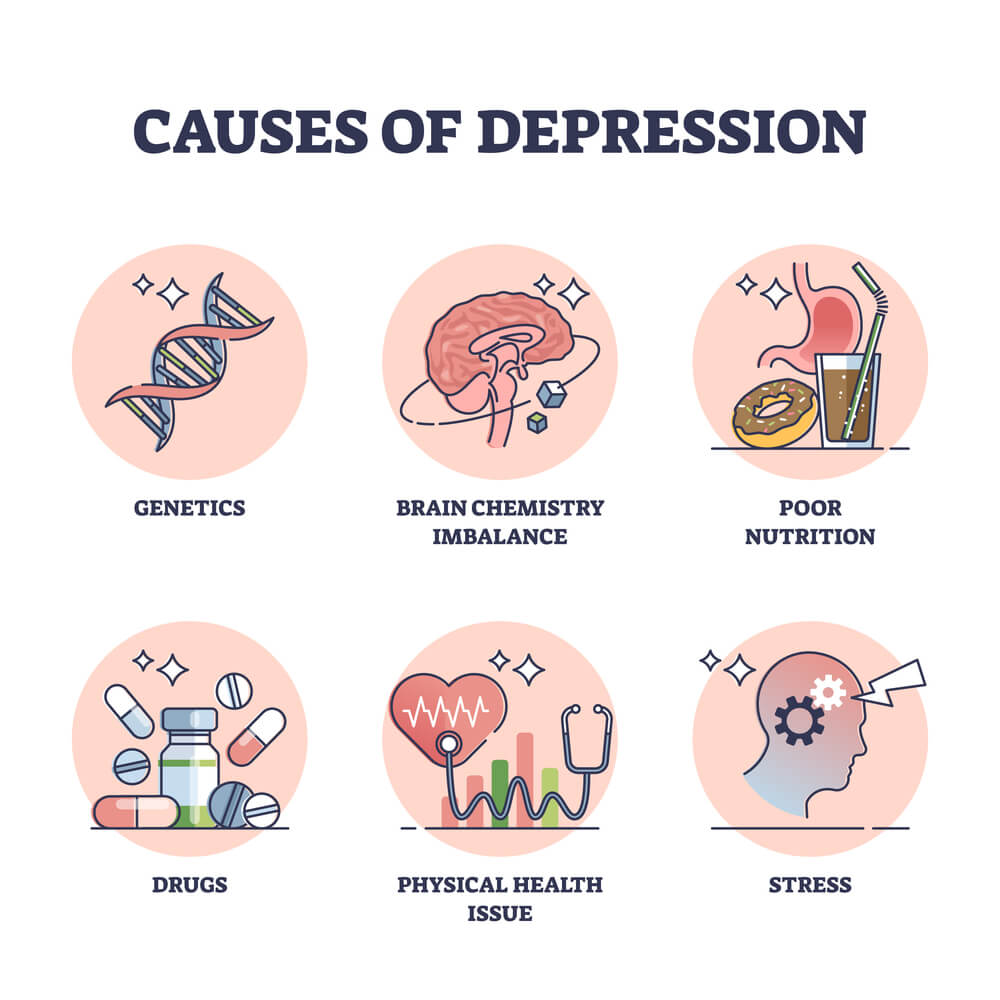
Stress can be caused by a variety of factors, including:
- Work-related stress, such as job insecurity, long hours, or a heavy workload
- Financial stress, such as debt or a lack of savings
- Relationship stress, such as conflict with a partner or family member
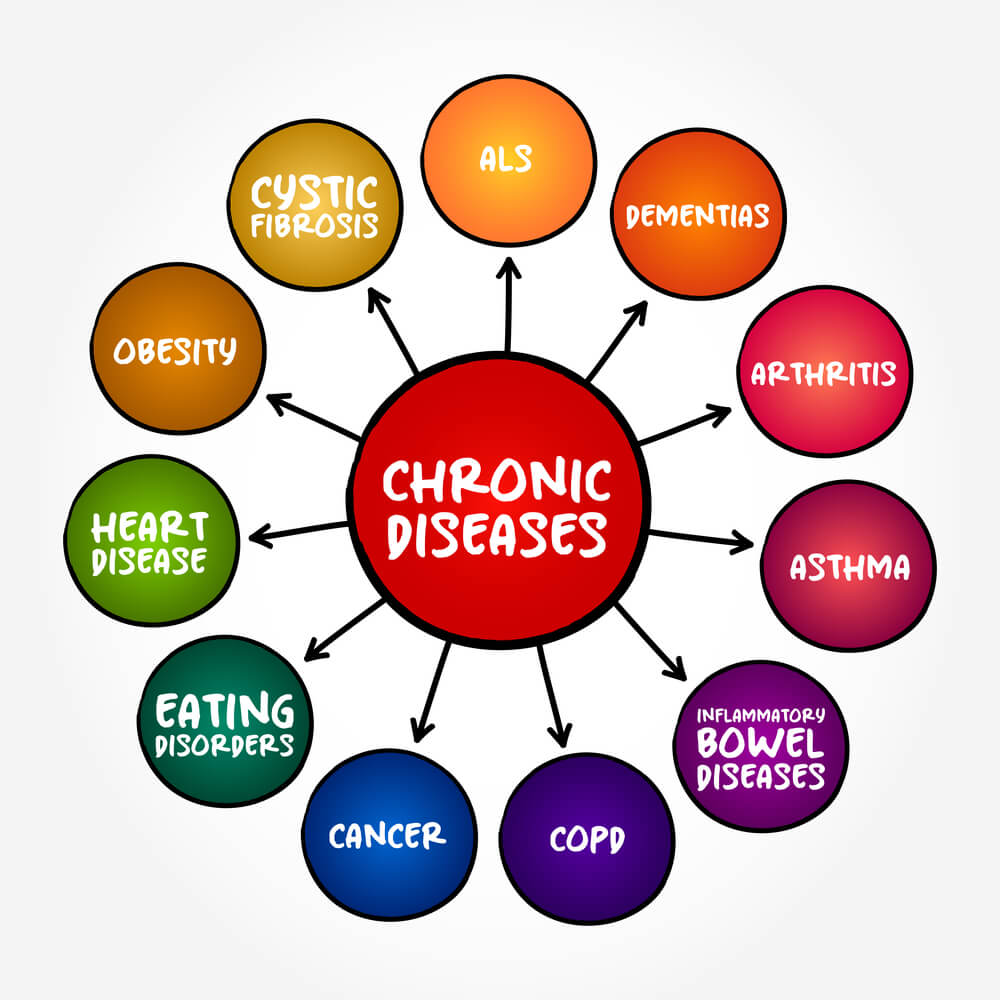
- Health-related stress, such as a chronic illness or injury
- Life changes, such as a move, divorce, or the death of a loved one
Again, what may be stressful for one person may not be for another. It’s important to identify the specific causes of stress in your life so that you can take steps to manage it effectively.
In the next section, we will explore some strategies for managing stress and building resilience.
Assessing Your Stress Levels
Stress can manifest itself in various ways, and it can be challenging to identify when it is affecting you. However, it’s essential to assess your stress levels regularly to know when to take action. This section will explore some techniques to help you assess your stress levels.
Self-Assessment Tools
There are several self-assessment tools available online that can help you determine your stress levels. These tools usually consist of a series of questions that assess various aspects of your life, such as work, relationships, and health. The results can provide you with an overall picture of your stress levels and help you identify areas that need improvement.
One such tool is the Perceived Stress Scale (PSS) 1. This scale consists of ten questions that assess how stressful you perceive your life to be. Another tool is the Holmes and Rahe Stress Scale 2. This scale assesses the impact of significant life events on your stress levels.
Reflecting on Stress Triggers
Another way to assess your stress levels is to reflect on your stress triggers. Stress triggers can be anything that causes you to feel stressed, such as deadlines, conflict, or financial difficulties. Identifying your stress triggers can help you take action to reduce their impact on your life.
To reflect on your stress triggers, take some time to think about the situations that cause you to feel stressed. Consider the following questions:
- What situations make you feel stressed?
- How do you react to stress?
- Are there any patterns in your stress triggers?
By reflecting on your stress triggers, you can identify the situations that cause you the most stress and develop strategies to manage them better.
In conclusion, assessing your stress levels is essential to building resilience. By using self-assessment tools and reflecting on your stress triggers, you can identify areas that need improvement and take action to reduce stress in your life.
References:
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of health and social behavior, 24(4), 385-396.
- Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of psychosomatic research, 11(2), 213-218.
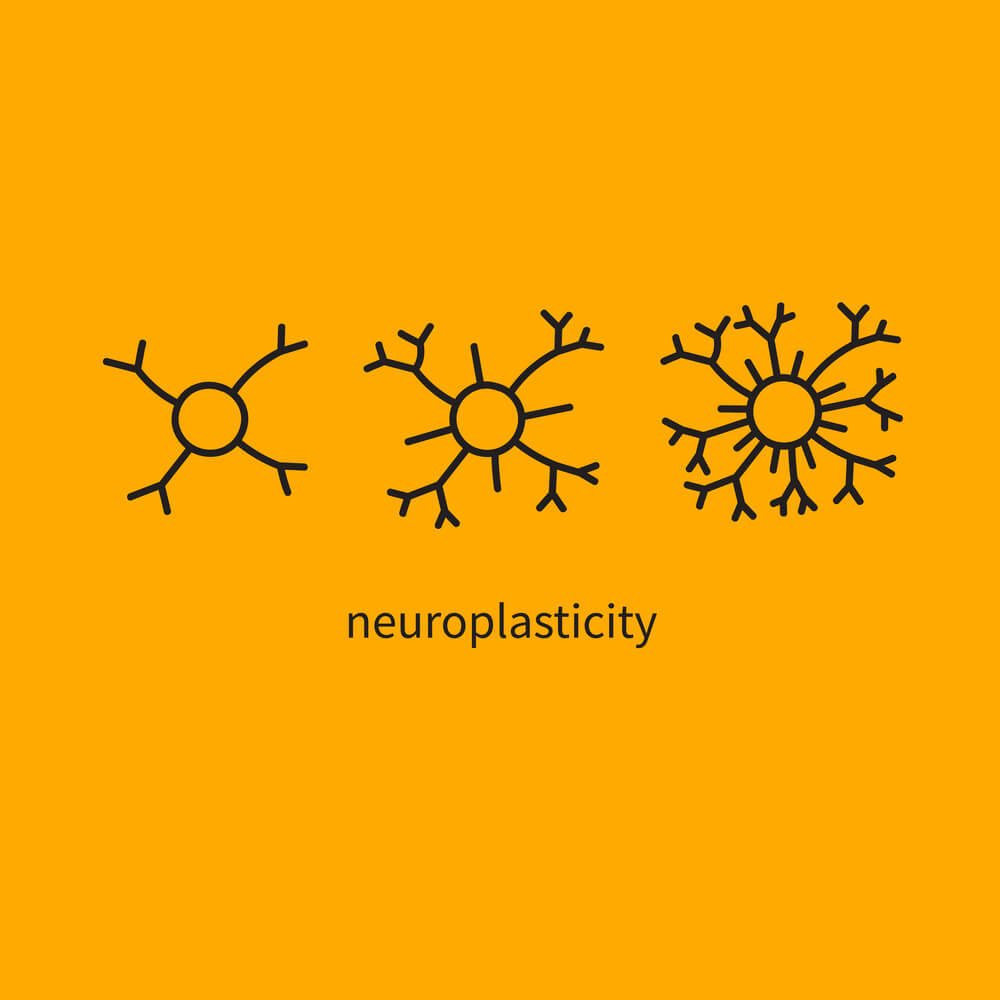
Building Resilience
Building resilience is an important skill that can help individuals cope with stress and adversity. Several strategies can help individuals build resilience, including developing a support network and using effective coping strategies.
Developing a Support Network
One effective way to build resilience is by developing a support network. This can include family, friends, coworkers, or a therapist. Having a support network can provide individuals with a sense of belonging and help them feel less alone during difficult times. It is important to prioritize relationships and focus on finding trustworthy and compassionate individuals who validate feelings, which will support the skill of resilience [1].
Effective Coping Strategies
Another way to build resilience is by using effective positive coping strategies. Coping strategies can include exercise, mindfulness, or engaging in hobbies. Developing interests and hobbies can help distract individuals from stressful situations. Spending time on things they enjoy could also help reduce stress and improve well-being [2].
In addition to developing a support network and using effective coping strategies, it is important to prioritize self-care and maintain a positive outlook. This can include getting enough sleep, eating a healthy diet, and practicing gratitude. By incorporating these strategies into their daily lives, individuals can build resilience and better cope with stress and adversity.
Implementing Stress Management Techniques
Mindfulness and Relaxation
One effective way to manage stress is through mindfulness practices such as meditation. This involves focusing your attention on the present moment and letting go of any distracting thoughts. Research has shown that regular mindfulness practice can reduce stress and anxiety levels.
Another relaxation technique is deep breathing exercises. This involves taking slow, deep breaths and focusing on your breath as it enters and leaves your body. This can help to calm your mind and reduce stress levels. I have heard that if you take 3 long slow breaths in through your nose and hold for 5 seconds before exhaling by pursing your lips and breathing out, you can calm your nervous system. Yes, it really does.
Time Management and Prioritization
Effective time management can also help to reduce stress levels. This involves prioritizing tasks and breaking them down into smaller, more manageable steps. Creating a to-do list and setting realistic deadlines can help to reduce feelings of overwhelm and increase productivity.
Another important aspect of time management is setting boundaries. This means learning to say no to tasks or commitments that are not essential or that will cause undue stress. It’s important to prioritize self-care and make time for activities that bring joy and relaxation.
By implementing these stress management techniques, individuals can build resilience and better manage stress in their daily lives.
Maintaining a Healthy Lifestyle
Maintaining a healthy lifestyle is an important part of building resilience and managing stress. In this section, we will discuss two key components of a healthy lifestyle: exercise and physical activity, and balanced diet and nutrition.
Exercise and Physical Activity
Regular exercise and physical activity can help reduce stress and improve overall well-being. Exercise releases endorphins, which are chemicals in the brain that act as natural painkillers and mood elevators. It also helps to reduce the levels of stress hormones in the body.
It is recommended that adults engage in at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, in addition to muscle-strengthening activities at least two days per week. This can include activities such as brisk walking, running, cycling, swimming, or strength training.
Balanced Diet and Nutrition
Eating a balanced diet and getting proper nutrition is also important for maintaining a healthy lifestyle and building resilience. A balanced diet should include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats.
It is important to limit the intake of processed foods, sugary drinks, and foods high in saturated and trans fats. These types of foods can increase inflammation in the body and contribute to chronic diseases such as heart disease, diabetes, and obesity.
In addition to eating a balanced diet, it is important to stay hydrated by drinking plenty of water throughout the day. Dehydration can lead to fatigue, headaches, and difficulty concentrating.
By incorporating regular exercise and physical activity and maintaining a balanced diet and proper nutrition, individuals can improve their overall health and well-being, and build resilience to stress.
Frequently Asked Questions
What are the signs of stress to look out for in your daily routine?
Stress can manifest itself in various ways, and it’s essential to recognize the signs to take appropriate action. Some common symptoms of stress include fatigue, irritability, anxiety, depression, difficulty sleeping, and physical symptoms such as headaches, muscle tension, and stomach problems. If you notice any of these symptoms, it’s crucial to take a step back and evaluate what might be causing the stress in your life.
What strategies can help increase emotional resilience in adults?
Emotional resilience is the ability to adapt and cope with stress and adversity. Some strategies that can help increase emotional resilience in adults include practicing mindfulness, building healthy relationships, engaging in physical activity, setting realistic goals, and seeking support from a mental health professional when needed. It’s essential to develop a toolbox of coping strategies that work for you and to practice them regularly to build resilience.
In what ways can resilience be strengthened within a workplace environment?
Resilience can be strengthened within a workplace environment by creating a culture that supports employee well-being and mental health. This can include offering resources such as an employee assistance program, providing opportunities for professional development and growth, promoting work-life balance, and fostering a supportive and inclusive work environment. Employers can also encourage employees to take breaks, prioritize self-care, and seek help when needed.
Can you provide examples of how resilience is demonstrated in mental health?
Resilience is demonstrated in mental health by the ability to adapt and cope with challenges and stressors. For example, a person with depression who is resilient may be able to maintain a positive outlook, seek help when needed, and engage in self-care activities such as exercise and socializing. A person with anxiety who is resilient may be able to manage their symptoms through coping strategies such as deep breathing, mindfulness, and seeking support from loved ones. Resilience is a crucial component of mental health and can help individuals navigate difficult times.