It isn’t just a severe headache. Info for those that don’t know.
March 23, 2022
Migraines not only affect the person that has them, it also affects their loved ones. Everyone’s emotional health and well-being are affected. Irritation, negative feelings and sometimes anger shows up. That is normal. The problems arise when we don’t deal with the irritation, negative feelings and anger appropriately.
Look, the person that has migraines does not want to have them. They are sometimes debilitating and their quality-of-life sucks. Remember, it is not just a severe headache, it is a brain disorder. I have been on both sides of this issue. I have only had three debilitating migraines in my life. I also have had many migraines that were annoyances and I have had some that you cannot think clearly for hours. When you can’t think clearly, it takes about four times as long to work on a project than it normally does. Sometimes, you can push through and sometimes you can’t. Sometimes, medications work and sometimes they don’t.
Triggers
I know what most of my triggers are and I can do a pre-emptive strike with over-the-counter and prescription meds when I feel the familiar pain beginning. I call it, the cocktail. I usually only have to take the cocktail once and the pain decreases to where I can function almost normally. The great thing about the cocktail, I use less medication overall. My migraines are acute. If they were chronic, then I would have to take preventative measures all of the time. Preventative measures include prescription medications, supplements, massage, running, walking, stretching, etc. As you can see, there are many things that may help with preventative measures. You have to find the group of things that will work for you. We will talk more about treatments and prevention next time.
I am thankful that I do not have chronic migraines. For those that do, I can empathize with you. I can also empathize with your family. It is hard on the family when you have plans and then a debilitating migraine flares-up. The plans go out the window or the one that is having the migraine flare-up is left at home. It sucks.
If someone is having a severe migraine, they probably should not be left alone. They should be watched. Why? Because they usually cannot get liquids or crackers safely on their own. A person that is having a severe migraine may be having neurological deficit problems and they could even have a stroke. If a person gets to status migrainosus (severe pain, lasting 3 days or more) they can have a stroke. They usually need to be in the hospital at this stage with a neurologist monitoring their condition.
As you can see, migraine is not just a bad headache. It takes the whole family working together to help get a handle on calming down migraine. Learning and understanding what a migraine disorder is and the ways in which each of you can help makes it much less stressful on all involved.
Eating nutritionally better, regular exercise, staying hydrated, learning more effective ways to deal with stress will help all involved. Help lighten the load at home for the one that has migraines. Be supportive. Ask how you can help them. Don’t be an ass. This is hard when you have been dealing with migraines for a while. During an attack is not the time to go through all the preventive measures “they should be doing.” Learning their own preventive measures takes time.
For those that have migraine flare-ups. Are you actively doing anything to try and find ways to decrease your attacks? Are you open to trying two or three things for 3 months to see if they help? Some of you have hurt for so long, that you don’t feel like you have the energy to find things that help. Maybe, you need help in getting plans of action that are unique to you and your needs.
**Shameless plug – I help with these types of plans. – Shameless plug over.**
If you have given up, I hope that you reconsider. Will you be open to the possibility that you can be helped? That you can get better and feel better? Yes, it will take time and effort on your part. You deserve to have fun and a good quality of life. If you are looking for an end to all the flare-ups and pain, that is not realistic, at this point in time. A decrease in migraine days and a decrease in the severity of pain is possible.
I encourage you to share this with others. Especially those that do not understand what happens during a migraine attack. My goal for this article is to help others better understand what a person that has migraines goes through.
Headache Types – Migraine, Non-migraine and Mixed
There are many types of headaches, about 150 different types. First, we have to figure out if the headache is a primary headache or a secondary headache. A primary headache has no known underlying cause. A secondary headache is the result of another condition. The other conditions are things like, inflammation, bacterial or viral infections, a trauma to the head or neck, sinusitis, etc.
Examples of the most common primary headaches:
-
- Cluster headache
-
- Migraine (with and without aura)
-
- Tension headache (medically known as tension-type headache)
-
- Trigeminal autonomic cephalalgia (TAC), including cluster headache and paroxysmal hemicrania
-
- Silent migraine
-
- Basilar migraine
-
- Abdominal
-
- Ocular
-
- Vestibular
-
- Status Migrainosus – ongoing pain lasting for more than 3 days
Examples of the most common secondary headaches related to another medical condition:
-
- Disease of blood vessels in the brain
-
- Head injury
-
- High blood pressure (hypertension)
-
- Infection
-
- Medication overuse
-
- Sinus congestion
-
- Trauma
-
- Tumor
-
- Hangover
-
- Menstrual
-
- Exertional
There is a mixed type of headache, a migraine and a tension type headache that happen at the same time. Some call it a mixed tension migraine.
A migraine can occur in four different phases. Not everyone will experience every phase.
Premonitory phase – also known as the prodrome phase
Non-painful symptoms that may occur a few hours of a few days Before the headache arrives.
-
- Unexplained mood changes
-
- Food cravings
-
- Neck stiffness
-
- Increased yawning
-
- Diarrhea or Constipation
-
- Increased sensitivity to light, sound, or smells
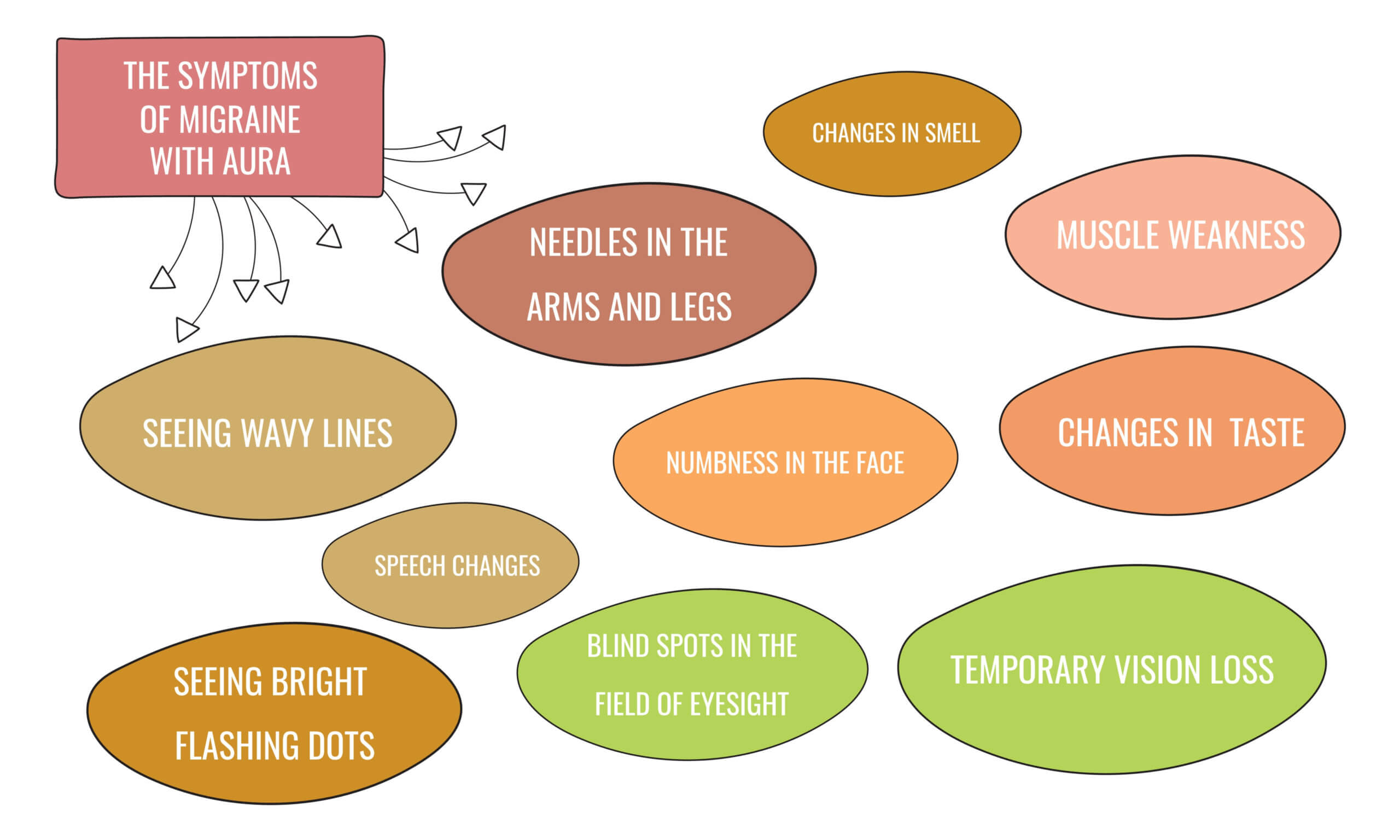
Aura phase – sensory disturbances that may occur before or during an attack
Visual auras may occur in one or both eyes
-
- flashing lights
-
- zig-zagging lines
-
- blurred vision
-
- blind spots that expand over time
Sensory auras cause numbness or tingling that starts in the arm and radiates to the face.
Motor auras cause problems in the person’s ability to think clearly and communicate verbally.
-
- slurred or jumbled speech
-
- difficulty understanding what others say
-
- difficulty writing words or sentences
-
- having trouble thinking clearly
Headache phase – pain ranges from mild to sever (not everyone will have a headache, but they may have all of the other symptoms such as nausea, vomiting, off balance, etc.
Postdrome phase – happens after the headache subsides and lasting a few hours to a few days
-
- exhaustion
-
- confusion
-
- generally feeling like crap
Migraine Triggers:
-
- lack of sleep or jet lag
-
- hunger or dehydration
-
- foods
-
- additives
-
- alcohol
-
- caffeine
-
- medication overuse
-
- smells
-
- lights and sounds
-
- weather
-
- female hormones
-
- physical activity
- stress
Unusual signs and symptoms of migraine:
-
- Body chills
-
- Phantom smells
-
- Brain fog
-
- Insomnia
-
- Stuffy or Runny nose
-
- Watery eyes
-
- Your skin or hair hurts – Allodynia – pain from things that do not normally hurt
-
- Hiccups
-
- Ringing in your ears
-
- Double vision
-
- Trouble hearing or understanding what others are saying
-
- Sparks of light in vision
The Complete Headache Chart
| Type | Symptoms | Precipitating Factors | Treatment | Prevention |
| Hangover Headaches | Migraine‐like symptoms of throbbing pain and nausea not localized to one side. | Alcohol, which causes dilation and irritation of the blood vessels of the brain and surrounding tissue. | Liquids (including broth). Consumption of fructose (honey, tomato juice are good sources) to help burn alcohol. | Drink alcohol only in moderation. |
| Caffeine‐ Withdrawal Headaches | Throbbing headache caused by rebound dilation of the blood vessels, occurring multiple days after consumption of large quantities of caffeine. | Caffeine. | In extreme cases, treat by terminating caffeine consumption. | Avoiding excess use of caffeine. |
| Exertion Headaches | Generalized head pain of short duration (minutes to 1 hour) during or following physical exertion (running, jumping, or sexual intercourse), or passive exertion (sneezing, coughing, moving one’s bowels, etc.). | 10% caused by organic diseases (aneurysms, tumors, or bloodvessel malformation). 90% are related to migraine or cluster headaches. | Cause must be accurately determined. Most commonly treated with aspirin, indomethacin, or propranolol. Extensive testing is necessary to determine the headache cause. Surgery to correct organic disease is occasionally indicated. | Alternative forms of exercise. Avoid jarring exercises. |
| Post‐Traumatic Headaches | Localized or generalized pain, can mimic migraine or tension‐type headache symptoms. Headaches usually occur on daily basis and are frequently resistant to treatment. | Pain can occur after relatively minor traumas. Cause of pain is often difficult to diagnose. | Possible treatment by use of antiinflammatory drugs, propranolol, or biofeedback. | Standard precautions against trauma. |
| Hunger Headaches | Pain strikes just before mealtime. Caused by muscle tension, low blood sugar, and rebound dilation of the blood vessels, oversleeping or missing a meal. | Strenuous dieting or skipping meals. | Regular, nourishing meals containing adequate protein and complex carbohydrates. | Same as treatment. |
| Temporomandibul ar Joint (TMJ) Headaches | A muscle‐contraction type of pain, sometimes accompanied by a painful “clicking” sound on opening the jaw. Infrequent cause of headache. | Caused by malocclusion (poor bite), stress, and jaw clenching. | Relaxation, biofeedback, use of bite plate. In extreme cases, correction of malocclusion. | Same as treatment. |
| Tic Douloureux Headaches | Short, jab like pain in trigger areas found in the face around the mouth or jaw. Frequency and longevity of pain varies. Relatively rare disease of the neural impulses; more common in women after age 55. | Cause unknown. Pain from chewing, cold air, touching face. If under age 55, may result from neurological disease, such as MS. | Anticonvulsants and muscle relaxants. Neurosurgery. | None. |
| Fever Headaches | Generalized head pain that develops with fever. Caused by swelling of the blood vessels of the head. | Caused by infection. | Aspirin, acetaminophen, NSAIDs, antibiotics. | None. |
| Arthritis Headaches | Pain at the back of head or neck. Intensifies on movement. Caused by inflammation of the blood vessels of the head or bony changes in the structures of the neck. | Cause of pain is unknown. | Anti‐inflammatory drugs, muscle relaxants. | None. |
| Eyestrain Headaches | Usually frontal, bilateral pain, directly related to eyestrain. Rare cause of headache. | Muscle imbalance. Uncorrected vision, astigmatism. | Correction of vision. | Same as treatment. |
| Temporal Arteritis | A boring, burning, or jabbing pain caused by inflammation of the temporal arteries. Pain, often around ear, on chewing. Weight loss, eyesight problems. Rarely affects people under 50. | Cause is unknown. May be due to immune disorder. | Steroids after diagnosis. Confirmed by biopsy. | None. |
| Tumor Headache | Pain progressively worsens, projectile vomiting, possible visual disturbances speech or personality changes; problems with equilibrium, gait, or coordination; seizures. Extremely rare condition. | Cause of tumor is usually unknown. | If discovered early, treat with surgery or newer radiological methods. | None. |
| Tension‐Type Headaches | Dull, non‐throbbing pain, frequently bilateral, associated with tightness of scalp or neck. Degree of severity remains constant. | Emotional stress. Hidden depression. | Rest, aspirin, acetaminophen, ibuprofen, naproxen sodium, combinations of analgesics with caffeine, ice packs, muscle relaxants. Antidepressants if appropriate, biofeedback, psychotherapy. If necessary, temporary use of stronger prescription analgesics. | Avoidance of stress. Use of biofeedback, relaxation techniques or antidepressant medication. |
| Migraine without Aura | Severe, one‐sided throbbing pain, often accompanied by nausea, vomiting, cold hands, sensitivity to sound and light. | Certain foods, the Pill or menopausal hormones, excessive hunger, changes in altitude, weather, lights, excessive smoking, and emotional stress. Hereditary component. | Ice packs; isometheptene mucate, combination products containing caffeine, ergotamine, DHE injectable and nasal spray, 5‐HT agonists; analgesics or medications, which constrict the blood vessels. For prolonged attacks steroids may be helpful. | Biofeedback, betablockers (propranolol, timolol), anti‐convulsant (divalproex sodium). Calcium blockers and NSAIDs may prevent or treat migraine headaches. |
| Migraine with Aura | Similar to migraine without aura, except warning symptoms develop. May include visual disturbances, numbness in arm or leg. Warning symptoms subside within one‐half hour, followed by severe pain. | Same as migraine without aura. | At earliest onset of symptoms, treat using biofeedback, ergotamine, dihydroergotamine or a 5‐HT agonist. Once pain has begun, treatment is identical to migraine without aura. | Prevent with same techniques as migraine without aura. |
| Cluster Headaches | Excruciating pain in vicinity of eye. Tearing of eye, nose congestion, flushing of face. Pain frequently develops during sleep and may last for several hours. Attacks occur every day for weeks/month, then disappear for up to a year. 80% of cluster patients are male, most ages 20‐50. | Alcoholic beverages, excessive smoking. | Oxygen, ergotamine, sumatriptan or intranasal application of local anesthetic agent. | Use of steroids, ergotamine, calcium channel blockers and lithium. |
| Menstrual Headaches | Migraine‐type pain that occurs shortly before, during, or immediately after menstruation or at mid‐cycle (at time of ovulation). | Variances in estrogen levels. | Same treatment as migraine. | Small doses of vasoconstrictors and/or anti‐inflammatory drugs before and during menstrual period may prevent headaches. Hysterectomy does not cure menstrual headaches. |
| Hypertension Headaches | Generalized or “hairband” type pain, most severe in the morning. Diminishes throughout day. | Severe hypertension: over 200 systolic and 110 diastolic. | Treat with appropriate blood pressure medication. | To prevent, keep blood pressure under control. |
| Aneurysm | Symptoms may mimic frequent migraine or cluster headaches, caused by balloon‐like weakness or bulge in blood‐vessel wall. May rupture (stroke) or allow blood to leak slowly resulting in a sudden, unbearable headache, double vision, rigid neck. Individual rapidly becomes unconscious. | Congenital tendency. Extreme hypertension. | If aneurysm is discovered early, treat with surgery. | To prevent, keep blood pressure under control. |
| Sinus Headaches | Gnawing pain over nasal area, often increasing in severity throughout day. Caused by acute infection, usually with fever, producing blockage of sinus ducts and preventing normal drainage. Sinus headaches are rare. Migraine and cluster headaches are often misdiagnosed as sinus in origin. | Infection, nasal polyps, anatomical deformities, such as a deviated septum, that block the sinus ducts. | Treat with antibiotics, decongestants, surgical drainage if necessary. | None. |
| Allergy Headaches | Generalized headache. Nasal congestion, watery eyes. | Seasonal allergens, such as pollen, molds. Allergies to food are not usually a factor. | Antihistamine medication; topical, nasal cortisone related sprays or desensitization injections. | None. |
Source: http://www.headaches.org/press/NHF_Press_Kits/Press_Kits_‐_The_Complete_Headache_Chart
Sometimes the dang chart does not completely transmit correctly, so you can use the link above.
Pat