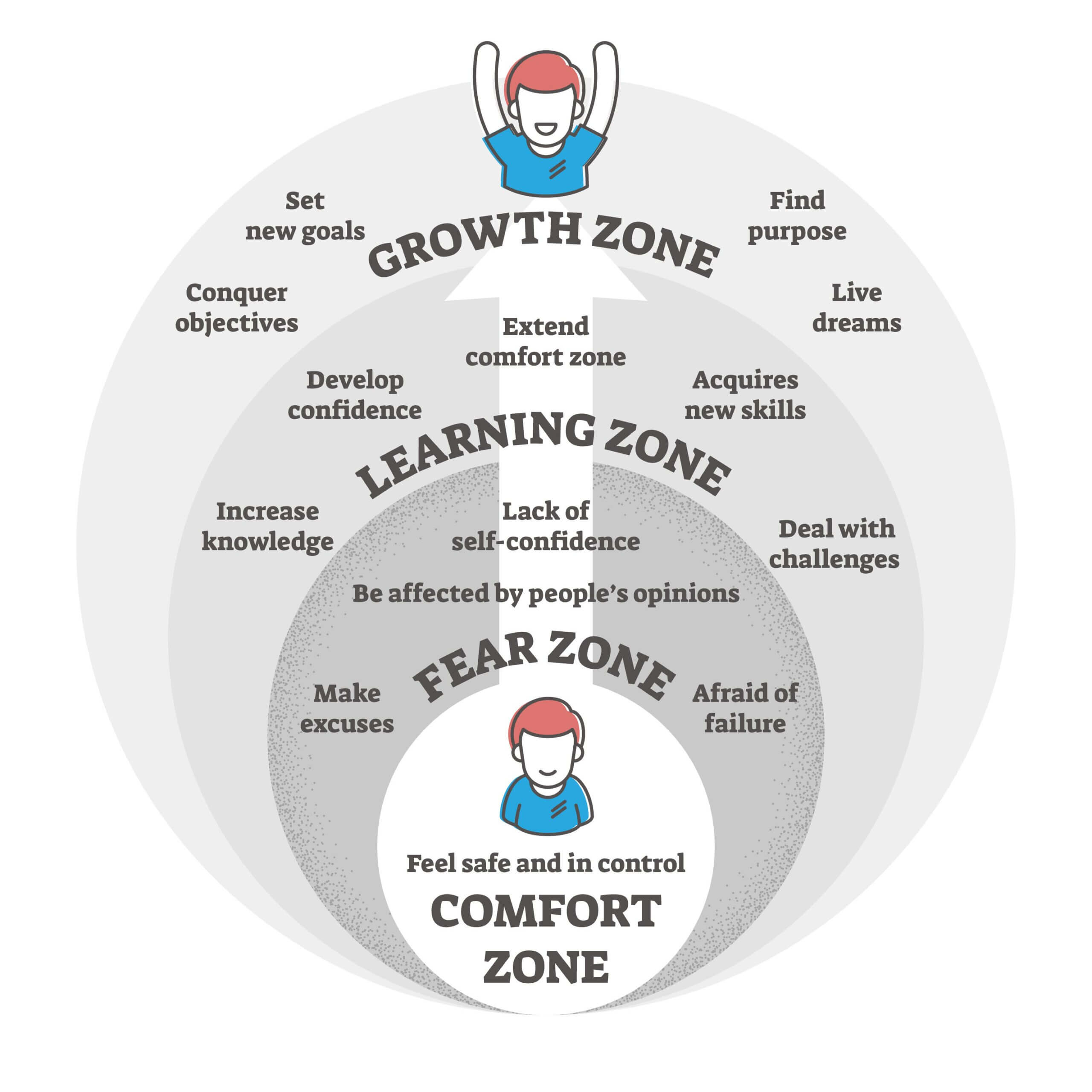
Sometimes, having a difficult conversation and being respectful don’t always go together. You can have a difficult conversation, but you can’t seem to reign in your emotions or you can talk about things that don’t really matter and be respectful. Think about it. How do you feel when you know a difficult decision must be made and you are facing a difficult conversation? Your heart begins to race, tension builds up in your body, and you are irritable. The conversation hasn’t even happened yet and you are all torn up.
You are on edge and ready for a fight. You don’t want to have this difficult conversation, but you’re facing it all the same. However, this is all in your mind. Nothing has happened, yet. Why do you feel this way? Past experience? Your racing thoughts are running amok and you are experiencing a stress response. You aren’t sure that a difficult conversation can be any other way than adversarial. Maybe, you don’t feel safe because you can’t predict the outcome.
March 15, 2023
First, let’s figure out what your style of communicating is when you are stressed. Yes, you handle things differently when you are at peace with yourself and your surroundings. Stress impacts our ability to communicate. What toll are your relationships taking when you are not at your best?
Self-awareness plays a vital role in this arena. Are you aware of how you are feeling and why you feel that way? Are you aware of when it is not a good time to have a difficult decision because you are not in the best frame of mind? Did you know that it is your responsibility to get your shit together and then have the hard talks?
When you are self-aware and emotionally healthy:
· You can intentionally respond to a situation. You think about the situation and act accordingly.
· You are more open to others’ ideas and inputs. You are looking for the best solutions.
· You are actually listening to understand and not just to respond.
· You are empathetic to the other person.
· You allow yourself to be curious about how the other person thinks and are open to changing your own mind.
· You will allow yourself to seek out support from others.
· You are willing to be understanding, supportive and fair.
· You have the ability to be patient during the discussion process.
When you are not emotionally healthy or self-aware:
· You tend to react to what the other person says and emotions escalate.
· You will be more critical of anything the other person is saying.
· You may even shut down and withdraw from the discussion.
· You tend to personalize the comments and do some projecting of how you feel onto the other person.
· You tend to be more judgmental and closed-minded.
· You will do things on your own and not seek out help or guidance from others.
· You will use manipulation, and verbal attacks to dominate the discussion.
· You are impatient and that will lead to you becoming pushy and interrupting.
When we are tired, we can slide into the not-emotionally healthy or self-aware category. What is usually a small annoyance can become a mega monster deal to us and we react accordingly. Notice that I said, react. We are not being rational or acting in the best manner. Our brains have been hijacked by the amygdala (stressors and cortisol dump) and we are off on a tear. What we sometimes forget is that there are people whom we love and care deeply for on the receiving end of those rants and raves.
So, what can we do to be in the best frame of mind when we need to have difficult conversations?
· Rest and get good sleep.
· Do something physical each day for 15-30 minutes.
· Write down 3 things that you are grateful for every day. Different things.
· Be aware of what your inner critic is saying to you. Is it true or correct? If not, then you have to get verbal with the inner critic and tell it to shut up. Your inner critic needs a new job but that is another discussion.
· You may not be able to rid yourself of stress, but you can manage your stress. Hopefully, you will do that in constructive ways.
We can all benefit from learning how to become better communicators. Take a course, do a seminar, or look up good articles online.
Our scenario:
Let’s look at the driving issue that seems to pop up. Here is the situation. Your dad needs to stop driving. He no longer has quick enough reflexes. His arthritis and neck issues are worse. Maybe there is some dementia that is now becoming an issue. You have noticed dings in the car on the sides and in the rear. The reasons could be physical, mental, or both.
You know that this is going to be difficult and it could get ugly. Hence, the stress response. You also know that this very difficult conversation has to happen soon because you are truly concerned for their safety and the safety of others.
Now that you have the scenario, what is the best approach for you to use when this discussion has to happen and you want to be helpful, loving, and respectful?
Family dynamics will play a part in this. It is best for the person who will have more sway with them to do the talking. This is not a guarantee, but it will help. Keep the main thing the main thing. Don’t get off-topic and into the weeds. Know what your “main thing” is. Next, you will need to state the “why’s.”
The main thing – stop driving
Why’s –
§ Cognitive decline (dementia, Alzheimer’s disease, or other impairment)
§ Problems with mobility or coordination
§ Vision problems
§ Hearing loss
§ Sleep disorder
§ Seizures
§ Inability to turn their head and neck very far
All right, you have your main thing and your “why’s.” Now you need to prepare for the emotions that will come from you and them. This is where you discuss and listen with respect. That means no name-calling, no cussing, no threatening, no bulldozing over their concerns or pushback.
They are going to push back. They are going to fight you on this. The best way to prepare for this is to listen to what their concerns are and understand what they are trying to say. I guarantee you that there are many things not being said and that is the real problem. Understand the other person’s point of view. Keep the conversation going as long as it is productive and emotions don’t send it off the rails.
What is not being said is, “I don’t want to give up my independence.”
“I want to go and do as I please.”
“I don’t want to bother you or be a burden.”
“I don’t want you judging me for where I go or what I do.”
“I am your dad, you are not my dad.”
“I will not be told what I can and cannot do.”
Take the time to understand things from their point of view. Imagine yourself being in the same situation because you’re going to be in the same situation one day so put yourself in their shoes.
You can keep stating the facts. You can even talk about the concerns you have for their safety, their passenger’s safety, or someone else’s safety. All of that is great and necessary. You have not addressed their concerns and wants. How will you handle that? You have to listen to the other person’s perspective.
You have to meet their needs and help them with what concerns them about not driving. Who will take them to the store, to the mall, to breakfast or lunch with friends? Who will take them to play golf, bowl, or to a ball game? Can they use a driving service such as a Taxi, Uber, or Lyft? Will you set up the drive to and from for them? Who will pay?
Whew! You may or may not have a resolution, yet. You may have to table this discussion until a later date. You may, in fact, have to have this discussion multiple times before a resolution is reached. Unless they have a cognitive impairment, you may never get them to stop driving. Their doctor may have more sway than you and that is fine to use the doctor if needed. You can’t make someone do or not do anything. They get to make the decision, even if it is a bad decision.
The purpose of this exercise was to show you an example of a difficult discussion and some things to think about before jumping in. To show you that you can prepare, you can listen for understanding and provide alternative solutions to meet their needs.
You are in control and in charge of your own emotions, feelings, and how to act and react. You are not in control of any other person’s actions or reactions.
A few tips:
· Use “I” statements. Do not use any sentence that starts with ”you.” It makes people defensive.
· Do not be sarcastic.
· Do not use the words, “always” or “never”
· Look at them in the eye.
· Do not interrupt them. Let them say what they need to say.
· Stick to their abilities and not their age.
· Remember to value the relationship.
· Be solutions-oriented. Ask them to be solutions-oriented.
· Watch your tone.
· Remember to deep breathe.
· It is okay to disagree. Maybe a neutral person needs to do an evaluation of driving skills.
· Have them drive you around.
· Maybe, they can drive short distances in the mornings or early afternoons (avoid rush hours).
· Know when to start or not start the conversation. Is this the best time to have this discussion? What else is going on? The time may never be perfect, but you need to find the best time possible.
· Remember your purpose in having this difficult decision. You want them and others to be safe.
With any difficult discussion, emotions run high. Do what you can do to be prepared. Maintain your composure and learn to listen for understanding.
What disrespect looks like and sounds like
· Disrespectful people do not care about the other person’s feelings.
· People stop talking when you enter a room.
· They do not accept responsibility when both of you share some of the blame.
· They continuously interrupt you.
· Angry or rude outbursts
· Bullying
· Shaming you
· Arrogant behavior
· Sarcasm or Taunting
· Sighing, Making faces, Eye rolling
· The silent treatment
· Dismissing ideas without listening to them
You can become a more effective communicator. You can have difficult discussions with less stress. You can do all these things. You can learn better communication strategies. You know what you want to accomplish. Are you also willing to agree to disagree and improve the situation?
Pat