Motivation is a crucial factor in achieving success in any aspect of life, yet it is something that often fails us. Many people struggle with motivation, whether it be for work, exercise, or personal goals. Understanding why motivation fails and what can be done about it is essential for anyone looking to achieve their goals.
One reason why motivation fails is that people often set unrealistic goals for themselves. When goals are too lofty, it can be difficult to maintain motivation over a long period of time. It is important to set achievable goals and to break them down into smaller, more manageable steps. This can help to maintain motivation and prevent burnout.
Another reason why motivation fails is that people often lack a clear sense of purpose. When people don’t have a clear understanding of why they are doing something, it can be difficult to maintain motivation. It is important to have a clear sense of purpose and to remind oneself of that purpose when motivation wanes. By understanding why motivation fails and what can be done about it, individuals can take steps to maintain their motivation and achieve their goals.
Understanding Motivation
Motivation is the driving force behind human behavior. It is what makes us get up in the morning, go to work, and pursue our dreams. However, sometimes motivation fails, and we find ourselves struggling to get things done. In this section, we will explore the psychology of motivation and the different types of motivation.
The Psychology of Motivation
According to Psychology Today, motivation is the desire to act in service of a goal. It is the crucial element in setting and attaining our objectives. Motivation is one of the driving forces behind human behavior, and it fuels our actions.
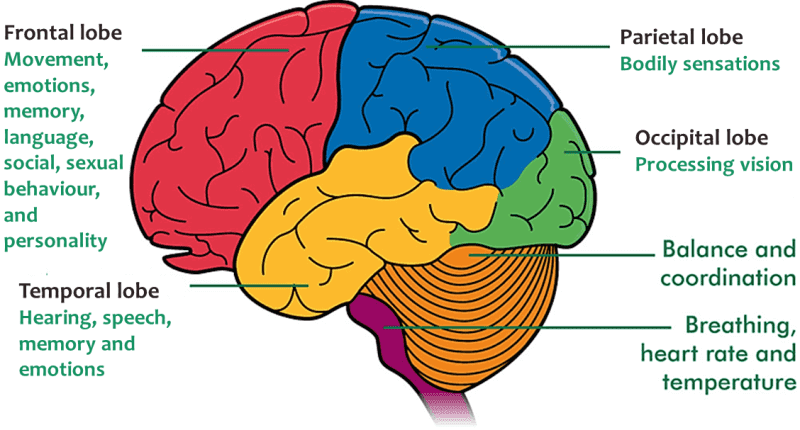
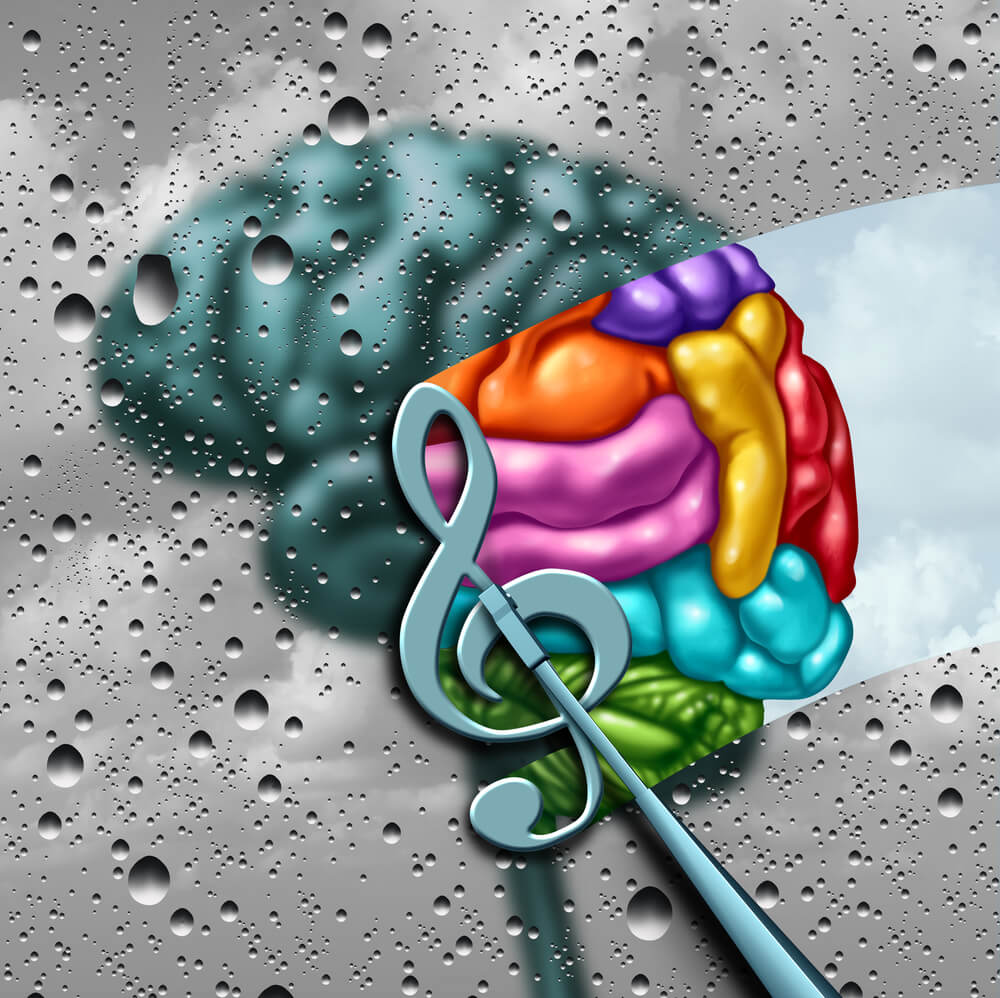
The psychology of motivation is complex, and there are many factors that can impact our motivation levels. One of the key factors is the reward system. When we receive a reward for our actions, our brains release dopamine, which makes us feel good. This positive feeling reinforces our behavior and motivates us to continue.
Another factor that can impact motivation is the level of challenge. If a task is too easy, it can be boring, and we may lose motivation. On the other hand, if a task is too difficult, it can be overwhelming, and we may give up. Finding the right level of challenge is important for maintaining motivation.
Types of Motivation
There are two main types of motivation: intrinsic and extrinsic. Intrinsic motivation comes from within, and it is driven by personal satisfaction and enjoyment. For example, someone who loves playing the piano may be intrinsically motivated to practice every day.
Extrinsic motivation, on the other hand, comes from external factors, such as rewards or punishments. For example, a student who studies hard to get good grades is extrinsically motivated.
While both types of motivation can be effective, research has shown that intrinsic motivation is more sustainable in the long run. When we are intrinsically motivated, we are more likely to enjoy the process and continue pursuing our goals, even when external rewards are not present.
Understanding the psychology of motivation and the different types of motivation can help us identify why our motivation may be failing and what we can do to get back on track.
Common Causes of Motivation Failure
Motivation can be a fickle thing. One day, you’re raring to go, and the next, you can’t seem to muster the energy to get out of bed. But why does motivation fail, and what can you do about it? Here are some common causes of motivation failure:
Lack of Clear Goals
One reason motivation can falter is a lack of clear goals. When you’re not sure what you’re working toward, it’s hard to stay motivated. Without a clear sense of direction, it’s easy to get sidetracked or lose focus. To combat this, it’s essential to set specific, measurable goals. Write them down and make a plan for how you’ll achieve them. Having a roadmap can help keep you on track and motivated.
Fear of Failure
Another common cause of motivation failure is fear of failure. When you’re afraid you won’t succeed, it’s hard to find the motivation to even try. This fear can be paralyzing and prevent you from taking risks or pursuing your goals. To overcome this, it’s important to reframe failure as a learning opportunity. Failure is not the end of the world; it’s a chance to grow and improve. By embracing failure as part of the process, you can find the motivation to keep going.
Burnout and Overwhelm
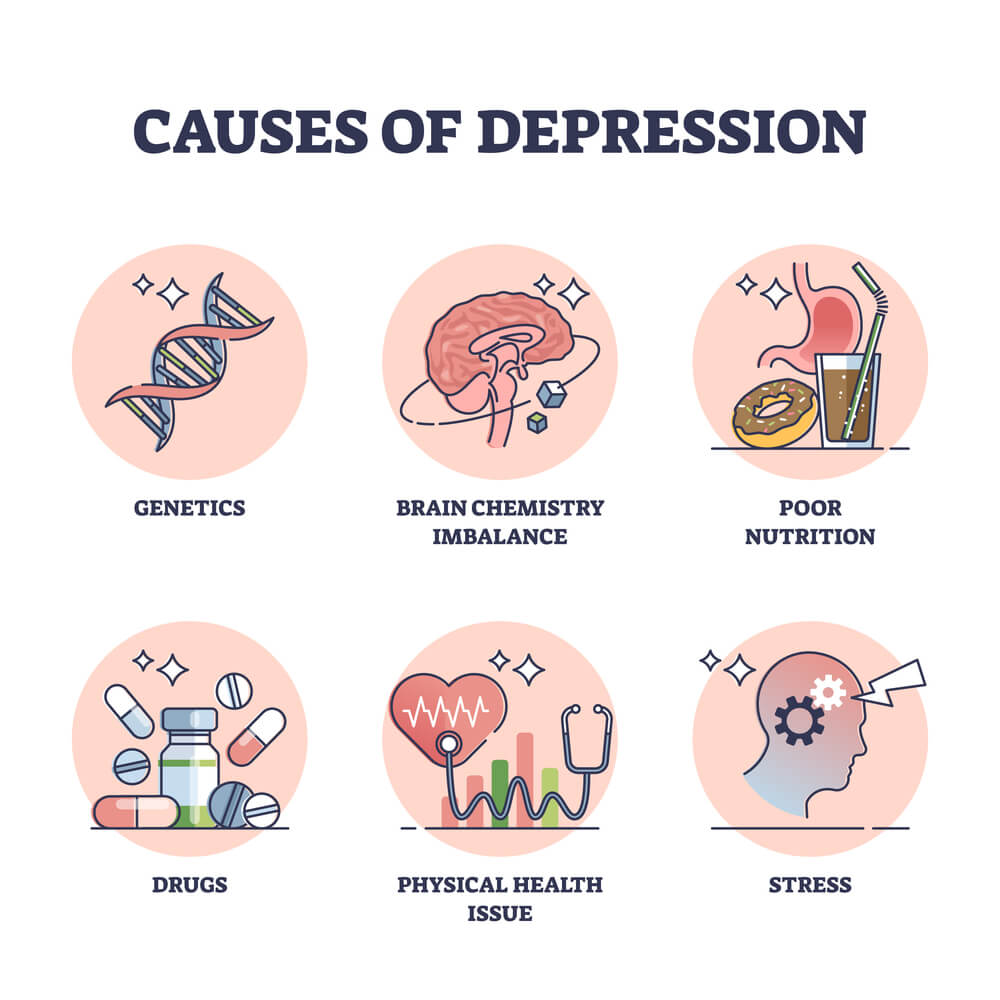
Finally, burnout and overwhelm can be major contributors to motivation failure. When you’re stretched too thin and feel like you can’t keep up, it’s easy to lose motivation. Burnout can leave you feeling exhausted, emotionally drained, and unmotivated. To combat burnout, it’s important to take breaks, prioritize self-care, and set boundaries. By taking care of yourself, you can recharge your batteries and find the motivation to keep going.
Strategies to Enhance Motivation
Motivation can be a fickle thing. Sometimes, even the most motivated individuals can find themselves struggling to stay on track. However, there are a few strategies that can help enhance motivation and keep individuals focused on their goals.
Setting Achievable Goals
One of the most important strategies for enhancing motivation is setting achievable goals. When individuals set goals that are too lofty or unrealistic, they may become discouraged and lose motivation. Instead, they should set small, achievable goals that can be accomplished in a reasonable amount of time. This can help build momentum and keep motivation levels high.
Creating a Support System
Another important strategy for enhancing motivation is creating a support system. Having a network of supportive individuals can make a big difference in keeping motivation levels high. Whether it’s a friend, family member, or coworker, having someone to talk to and share progress with can help keep individuals accountable and motivated.
Incorporating Rewards and Recognition
Finally, incorporating rewards and recognition can also be an effective strategy for enhancing motivation. When individuals have something to look forward to, such as a reward for meeting a goal, they are more likely to stay motivated. Additionally, recognition for a job well done can help boost morale and keep individuals focused on their goals.
Overall, enhancing motivation requires a combination of strategies. By setting achievable goals, creating a support system, and incorporating rewards and recognition, individuals can stay motivated and focused on achieving their goals.
Overcoming Internal Barriers
When it comes to motivation, sometimes the biggest obstacles are the ones we create for ourselves. These internal barriers can be difficult to overcome, but with the right strategies, it is possible to break through them and achieve your goals.
Challenging Negative Beliefs
One of the most common internal barriers to motivation is negative self-talk. When you tell yourself that you can’t do something or that you’re not good enough, it becomes much harder to take action and make progress. To overcome this barrier, it’s important to challenge these negative beliefs and replace them with more positive and empowering ones.
One way to do this is to keep a journal of your thoughts and feelings. Whenever you notice negative self-talk, write it down and then challenge it. Ask yourself if it’s really true or if there’s evidence to the contrary. Then, come up with a more positive and realistic thought to replace it with.
Another strategy is to surround yourself with positive and supportive people. Seek out friends, family members, or colleagues who will encourage you and help you stay motivated. You can also join a support group or online community where you can connect with others who share your goals and struggles.
Building Self-Discipline
Another internal barrier to motivation is a lack of self-discipline. When you struggle to stick to a routine or follow through on your commitments, it can be hard to make progress towards your goals. To overcome this barrier, it’s important to develop your self-discipline and willpower.
One way to do this is to set small, achievable goals and then work towards them consistently. Start with something simple, like drinking more water each day, and then gradually increase the difficulty of your goals. This will help you build momentum and develop the habit of taking action.
Another strategy is to create a routine or schedule for yourself. This can help you stay on track and avoid procrastination. Make sure to include breaks and rewards in your schedule to help you stay motivated and avoid burnout.
By challenging negative beliefs and building self-discipline, it is possible to overcome internal barriers to motivation and achieve your goals. With persistence and dedication, anyone can develop the mindset and habits needed to succeed.
Sustaining Long-Term Motivation
Motivation is essential for achieving long-term goals, but it’s not always easy to maintain. Many people start with a burst of enthusiasm, but as time goes on, their motivation wanes. This can be particularly challenging when working on long-term projects or goals that require sustained effort. In this section, we will explore some strategies for sustaining long-term motivation.
Maintaining Work-Life Balance
One of the biggest challenges people face when trying to sustain long-term motivation is maintaining a healthy work-life balance. It’s easy to get caught up in work and neglect other important aspects of life, such as family, friends, and hobbies. This can lead to burnout and a loss of motivation.
To avoid this, it’s important to set aside time for activities outside of work. This can include spending time with loved ones, pursuing hobbies, or just taking some time to relax. By maintaining a healthy work-life balance, people can avoid burnout and stay motivated over the long term.
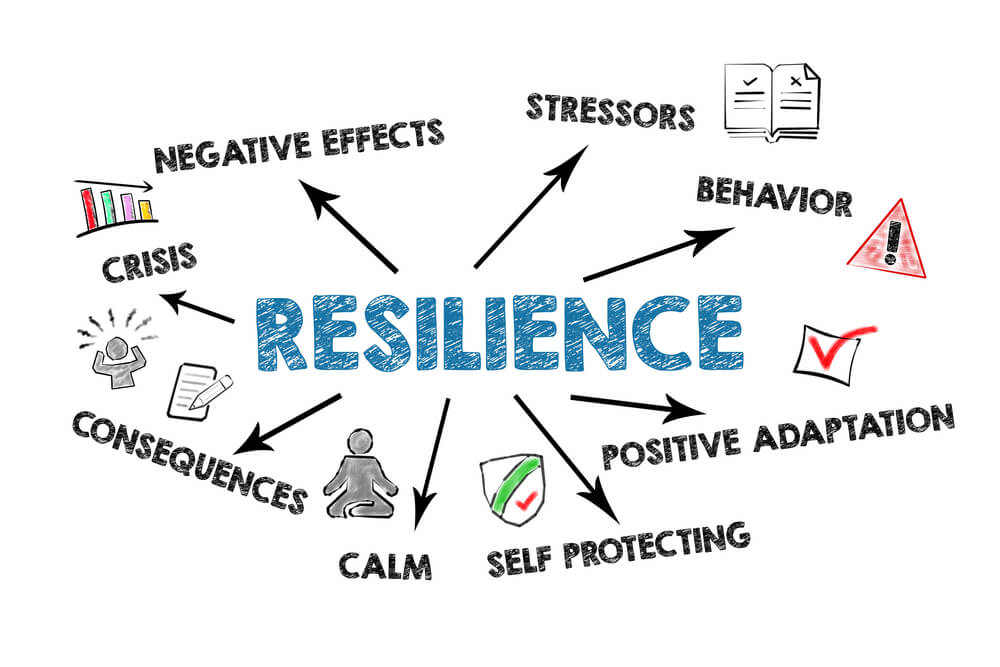
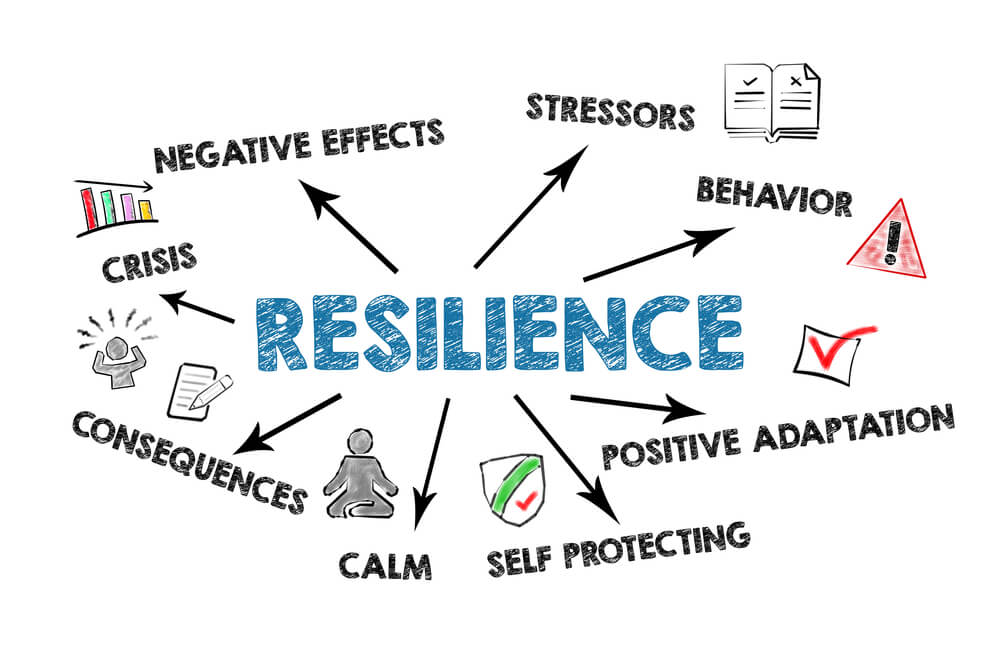
Adapting to Change and Setbacks
Another challenge people face when trying to sustain long-term motivation is adapting to change and setbacks. Life is full of unexpected twists and turns, and it’s easy to get discouraged when things don’t go as planned.
To overcome this, it’s important to be flexible and adaptable. People should be willing to adjust their goals and plans as needed and be open to new opportunities. Additionally, it’s important to view setbacks as learning opportunities rather than failures. By learning from setbacks, people can grow and become even more motivated to achieve their goals.
In summary, sustaining long-term motivation requires maintaining a healthy work-life balance and adapting to change and setbacks. By following these strategies, people can stay motivated and achieve their long-term goals.
Frequently Asked Questions
How can I regain motivation when I feel completely unmotivated?
It can be challenging to regain motivation when you feel completely unmotivated. One strategy that can be helpful is to break your goals down into smaller, more manageable tasks. This can make your goals seem less overwhelming and more achievable. Additionally, finding an accountability partner or seeking support from friends or family can help you stay motivated and on track.
What strategies are effective for overcoming a sudden loss of motivation?
A sudden loss of motivation can be frustrating, but there are several strategies that can help. One effective strategy is to take a break and engage in a different activity that you enjoy. This can help you recharge and refocus. Additionally, setting short-term goals and rewarding yourself for achieving them can help you stay motivated and avoid burnout.
Why do I struggle to maintain motivation over time?
Maintaining motivation over time can be challenging, and there are several reasons why this may be the case. One common reason is that goals may become less meaningful or relevant over time. To combat this, it can be helpful to regularly revisit your goals and reassess their importance. Additionally, finding ways to make your goals more enjoyable or rewarding can help you stay motivated.
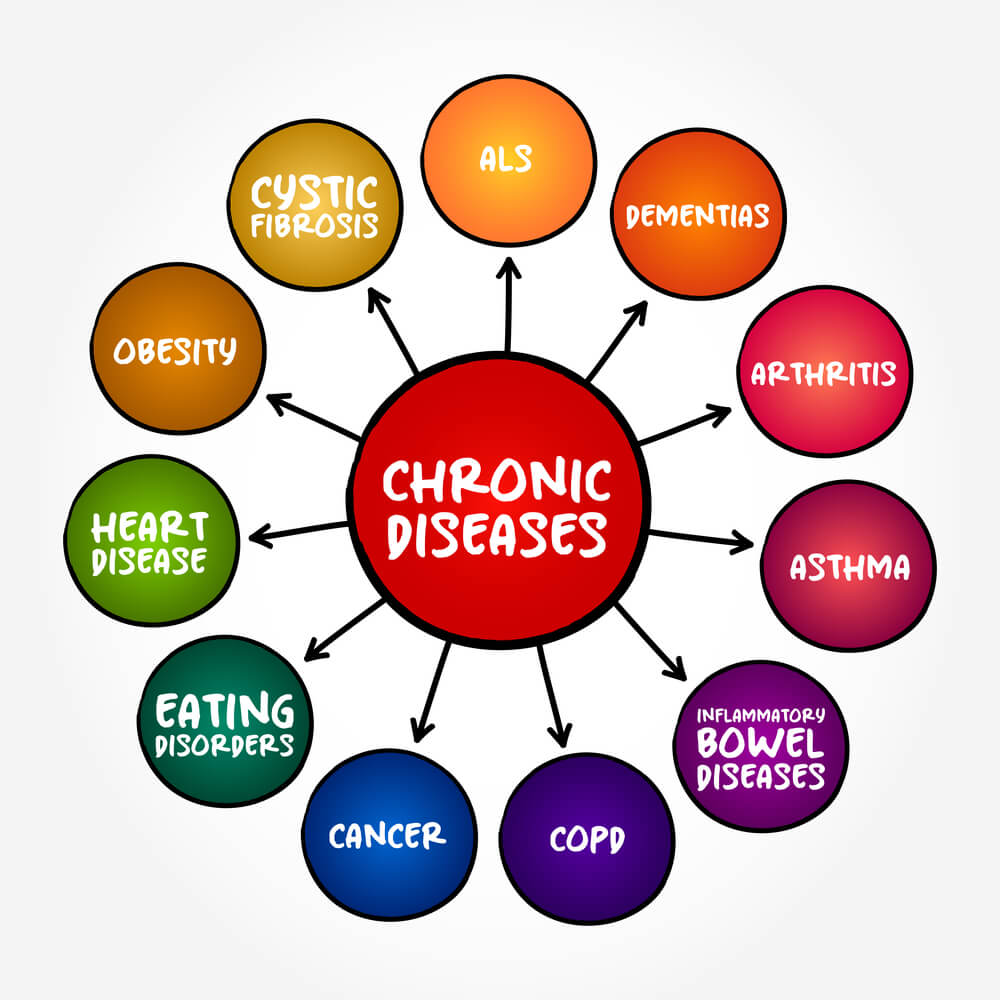
How can I motivate myself to take care of my well-being when I don’t feel like it?
Taking care of your well-being can be challenging, especially when you don’t feel like it. One strategy that can be helpful is to focus on the benefits of self-care and how it can improve your overall quality of life. Additionally, finding activities that you enjoy and that promote well-being, such as yoga or meditation, can help you stay motivated and engaged.
What causes a person to lose motivation for their studies or schoolwork?
Several factors can contribute to a loss of motivation for studies or schoolwork. One common factor is burnout, which can occur when a person is overworked or stressed. Additionally, lack of interest or relevance in the subject matter can also contribute to a loss of motivation. To combat this, it can be helpful to take breaks, seek support from teachers or peers, and find ways to make the subject matter more engaging.
Why do I have a lot of ideas but struggle to find the motivation to execute them?
Having lots of ideas can be exciting, but it can also be overwhelming. One reason why you may struggle to execute your ideas is that you may not have a clear plan or strategy for how to implement them. To combat this, it can be helpful to break down your ideas into smaller, more manageable tasks and create a timeline or roadmap for how to achieve them. Additionally, seeking support from others or finding an accountability partner can help you stay motivated and on track.