Think about it. Are you really having a conversation or are you just placating them so that you can get crap done? As the care giver or care partner are you even aware that your care receiver has needs that you can easily meet while you are handling tasks? I get it. A lot of us are task-oriented and do not want to be bothered with other things while we are doing our tasks. That would be great if our care receiver was not a human being. Take the time to talk with them.
September 14, 2022
When you are doing basic tasks
Most of the tasks you will be doing, will not take a lot of brain power or concentration. Let the stroke survivor help. Let the person with dementia help. Some tasks will take brainpower and you will need quiet time to concentrate, but not a lot of them. It does not take brain power or concentration to do laundry, wash dishes(place in or take out of dishwasher), cook something, sweep or mop, etc. You can be engaging your care receiver by talking, telling stories, or singing together. Paying bills, comparing EOB’s with medical bills and figuring things out, will take concentration and brain power. You do need quiet time for those types of things. To get that quiet time, engage your loved one before you get started. Take 10-15 minutes to be fully present with them.
Your loved one can sense your attitude
Remember, they can sense your attitude and feelings towards them even if they have any type of dementia. If they have a physical disability or injury, and they need a little help, they still like to be engaged in conversation or stay up-to-date with what is going on with you, the community, and the world. Let your loved one do whatever they can do, even if it takes three times as long.
We talk a lot about dementia patients, but let’s focus on care receivers that have a physical disability, such as stroke survivors. Stroke survivors need repetition and to continuously try things. It takes them longer but they can get better and better.
They need help and encouragement.
-
- Encourage them to do the exercises they have been given by their physical or occupational therapists. You have to rewire the brain and movement is key.
-
- Allow them to do what they can do, even if they struggle. Unless they ask for your help, let them keep working on it. Be helpful, but not overbearing.
-
- You may have access to a social worker or counselor, and use them for help and resources. An occupational therapist can help with identifying home modifications that would help.
-
- New stroke side effects may arise after going home. Be alert and contact their doctor.
-
- Understand that sometimes, the stroke survivor may have a little setback, before they move forward again.
-
- Always push past the plateau. There may be a time (3-6 months after a stroke) that “getting better” seems to level off. It may seem that way, but the brain is still healing and working. Keep on, keeping on. Changing exercises or rehab strategies may help, too.
-
- There may be emotional changes after a stroke. There may also be outbursts of laughing or crying due to pseudobulbar affect.
-
- Report falls to doctor
-
- Don’t give up, keep striving for the best. (Independence depends on this.)
As a care giver, learn as much as you can about your care receiver’s stroke. What areas of the brain were affected? What do those areas control? What to expect physically, emotionally and mentally.
Some of the symptoms that a stroke survivor may experience:
-
- Loss of control of movement &/or feeling in some parts of the body (This usually occurs on the side of the body opposite from the side of the brain affected.)
-
- Changes in muscle tone on the affected side of the body
-
- Involuntary muscle contractions
-
- Difficulty sitting, standing or walking
-
- Reduced ability to balance
-
- Problems with speaking and/or understanding speech
-
- Confusion and/or poor memory
-
- Decreased control over bladder, bowel or both
-
- Difficulty swallowing
-
- Reduced control over emotions
The following is from Johns Hopkins Medicine
What are the effects of stroke?
The effects of stroke vary from person to person based on the type, severity, location, and number of strokes. The brain is very complex. Each area of the brain is responsible for a specific function or ability. When an area of the brain is damaged from a stroke, the loss of normal function of part of the body may occur. This may result in a disability.
The brain is divided into 3 main areas:
-
- Cerebrum (right and left sides or hemispheres)
-
- Cerebellum (top and front of the brain)
-
- Brainstem (base of the brain)
Depending on which of these regions of the brain the stroke occurs, the effects may be very different.
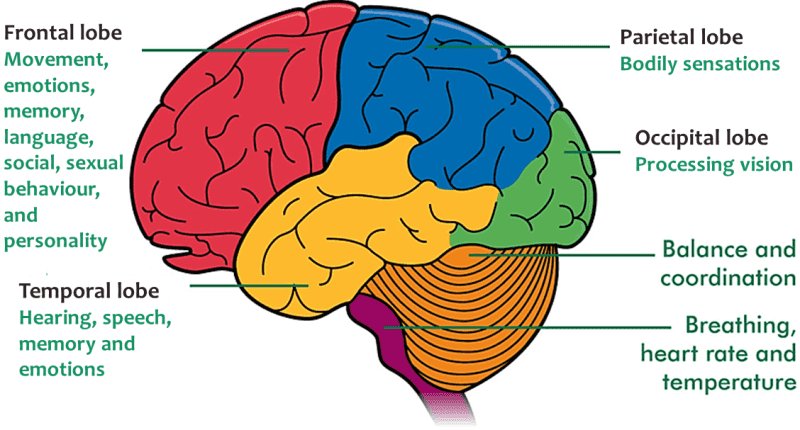
What effects can be seen with a stroke in the cerebrum?
The cerebrum is the part of the brain that occupies the top and front portions of the skull. It controls movement and sensation, speech, thinking, reasoning, memory, vision, and emotions. The cerebrum is divided into the right and left sides, or hemispheres.
Depending on the area and side of the cerebrum affected by the stroke, any, or all, of these functions may be impaired:
-
- Movement and sensation
-
- Speech and language
-
- Eating and swallowing
-
- Vision
-
- Cognitive (thinking, reasoning, judgment, and memory) ability
-
- Perception and orientation to surroundings
-
- Self-care ability
-
- Bowel and bladder control
-
- Emotional control
-
- Sexual ability
In addition to these general effects, some specific impairments may occur when a particular area of the cerebrum is damaged.
suffered a life-threatening stroke that left half her face paralyzed, a devastating loss for a talented
The effects of a right hemisphere stroke may include:
-
- Left-sided weakness or paralysis and sensory impairment
-
- Denial of paralysis or impairment and reduced insight into the problems created by the stroke (this is called “left neglect”)
-
- Visual problems, including an inability to see the left visual field of each eye
-
- Spatial problems with depth perception or directions, such as up or down and front or back
-
- Inability to localize or recognize body parts
-
- Inability to understand maps and find objects, such as clothing or toiletry items
-
- Memory problems
-
- Behavioral changes, such as lack of concern about situations, impulsivity, inappropriateness, and depression
The effects of a left hemisphere stroke may include:
-
- Right-sided weakness or paralysis and sensory impairment
-
- Problems with speech and understanding language (aphasia)
-
- Visual problems, including the inability to see the right visual field of each eye
-
- Impaired ability to do math or to organize, reason, and analyze items
-
- Behavioral changes, such as depression, cautiousness, and hesitancy
-
- Impaired ability to read, write, and learn new information
-
- Memory problems
What effects can be seen with a stroke in the cerebellum?
The cerebellum is located beneath and behind the cerebrum towards the back of the skull. It receives sensory information from the body through the spinal cord. It helps coordinate muscle action and control, fine movement, coordination, and balance.
Although strokes are less common in the cerebellum area, the effects can be severe.
Four common effects of strokes in the cerebellum include:
-
- Inability to walk and problems with coordination and balance (ataxia)
-
- Dizziness
-
- Headache
-
- Nausea and vomiting
What effects can be seen with a stroke in the brainstem?
The brainstem is located at the base of the brain right above the spinal cord. Many of the body’s vital “life-support” functions such as heartbeat, blood pressure, and breathing are controlled by the brainstem. It also helps control the main nerves involved with eye movement, hearing, speech, chewing, and swallowing.
Some common effects of a stroke in the brainstem include problems with:
-
- Breathing and heart functions
-
- Body temperature control
-
- Balance and coordination
-
- Weakness or paralysis
-
- Chewing, swallowing and speaking
-
- Vision
-
- Coma
Unfortunately, death is possible with brainstem strokes.
Over time, it may be harder for the stroke survivor to stay motivated during recovery. The two main contributors to this are apathy and depression. Apathy is a loss of motivation, concern, interest, and emotional response after a stroke. Feeling sad after a major life event that turns your world upside down is normal, depression seems to affect 30-50 percent of stroke survivors. Signs of depression include feelings of hopelessness and sadness that do not go away.
FYI – Help stroke survivors to stay motivated.
Set relevant and achievable goals
Address the emotional challenges and get help with medications and talk therapy
Help the stroke survivor understand about their stroke, the changes, the rehab, the plateau, etc.
Have a consistent routine, do it no matter how you feel about it
Find what motivates them
When motivation fails, discipline takes over – just do it
Pat

