Caregivers: How to manage multiple appointments
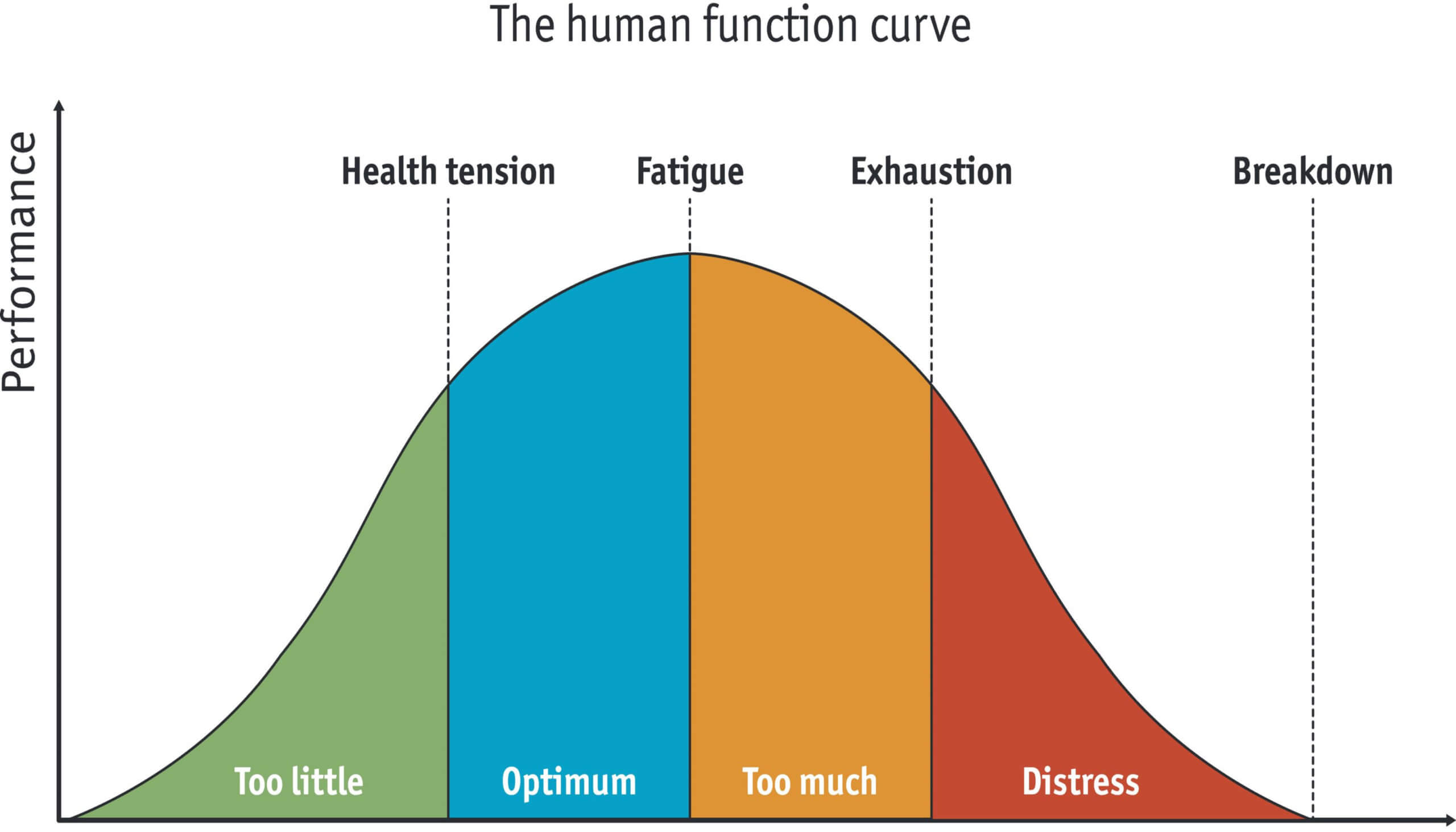
Sometimes, we are so stressed that we give up more of our power than we need to around scheduling. Sometimes, we are thrust in to a role without our prior permission. Other times, it is assumed that we will do X,Y or Z at A, B and C time and there is no way that we can make that work with our schedule. Talk about stress levels rising.
August 17, 2022
Get Legal Stuff in order for Caregiver
Before you are thrust in a role, have the tough conversations. Discuss who will be POA (power of attorney) for healthcare and for financial matters. It may or may not be the same person. It is much better to have these tough conversations with everyone who is to be involved, present at the meeting. No excuses, be there in-person, via telephone call or a Zoom meeting. Family caregiver supporters need this information.
Decide who will be the point person or the one with the overall knowledge of what is going on and what will need to happen. Next, we need volunteers to take loved one(s) to doctor appointments, therapy appointments, pharmacy pick-ups, grocery shopping, cleaning the house, barbershop appointments and hair dresser appointments.
Which family caregiver will do certain appts or emergency appts?
During an unexpected crisis or emergency, whoever is available or can take off, will have to step up and handle the appointment. Any time there is to be an initial appointment, you will probably have to take what you can get. After that, you can set the appointment day and time that works best for the patient and the companion or the driver. Decide what days and time are best for you to help your loved one. Maybe, you have one or two days during the week that are easier for you to take off work, come in late or leave early. Treatment Tuesdays, Wednesday Errands, Hair Thursdays, or Manic Mondays (get everything done on this day) are some examples. Caregiver support = helping caregivers with the care recipient.
Have a day for appointments and try for first appt.
Get the first appointment of the day, the appointment right after doctor’s lunch or the last appointment of the day. These are the most on-time appointments. Overall, most doctors are scheduling better and wait times are in the 20-minute range, if there is a wait time. Yes, your time is valuable and as you respect the doctor’s time by getting there 15 minutes early to check-in and update your information, if needed, your time needs to be respected as well.
I hear your voices in my head. The, “I had to wait 45 minutes passed the appointment time.” I get it , I have done it before too. I no longer do that. I give them 15 minutes and then I am back up at registration, checking out the situation. Oftentimes, you get back to a room at your scheduled time and then you have to wait for the doctor to come in. There is no easy solution with this type of situation. It could have been that two or three previous patients needed more time than what they were scheduled for. It could have been that the doctor got interrupted by an insurance company call. Before you get all pissed, give them the benefit of the doubt. There may come a time when you need more time with them and someone else will have to wait. You need a care team to provide care for your loved one.
Be prepared for your appointment
My appointments go smoothly because I am prepared. I get there 10 minutes early and check-in with insurance card and ID. Sign or fill out paperwork, if needed and I am ready to go. The assistant comes out and does the preliminary stuff. Takes down the notes for today’s visit and then I wait for my doctor. When he comes in, I have my list of medications out and ready. I have a list of meds that needs to be refilled ready to hand him. At the bottom of my list, are the 3 things that I want to talk about or have checked. If I am sick, I write down my symptoms in bullet points, how long it has been going on and what I have done or tried at home.
By the time he has read this, we are ready to discuss treatment options or next steps. He may have a few questions that need to be answered. I answer, he checks out what needs to be checked out, orders what lab tests needed and electronically sends off prescriptions to be filled at my pharmacy. We discuss whether a follow-up is needed and I am out the door.
Want respect? Give respect.
It is great to like your doctor and I hope that you do. Any good relationship is a mix of give and take. Do you want more respect, attention and help from your doctor? Then be prepared for your visit. They no longer have the time to shoot the breeze, they just don’t. I believe that they want to do a good job and help you. Remember, this is a business relationship. The business is your personal health. It is important and we all need a doctor that we can work with for our best quality of life.
On your sheet of paper list, the following:
-
- Current Medications, Why taking, Who prescribed it?
-
- Current over-the-counter (OTC) medications, herbal supplements, vitamins, etc.
-
- Chief complaint – what brought you to the doctor today?
-
- Signs & Symptoms you are having
-
- How long has this been going on?
-
- What have you tried or taken to help?
If you think your medications are not working or helping, state that and why you think that.
If you are having problems or unbearable side effects of your medications, tell your doctor.
If you haven’t been taking your medications, tell your doctor. What is the reason? Be honest.
Write out your questions
Write out your questions. I know that you think that you will remember, but you won’t. You will talk about everything else and then your appointment time will be over.
Stay focused on why you are there for that visit. There is such a thing as an extended visit, and maybe you need to ask for one of those for next time. If you have your all of your information and questions written down and ready, you may be surprised that you do have time left over.
Doctors like bullet points or statements of facts. Save the story for later, if you have time. Find out how the doctors like to be contacted. Email, leave a message, make an appointment, etc.
When mistakes happen
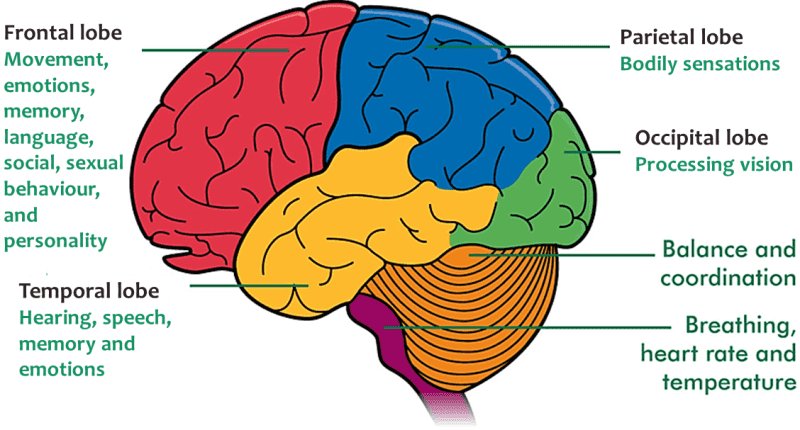
Mistakes happen. Things get dropped or missed. Yes, it is frustrating and sometimes maddening. Take a chill pill, your amygdala just hijacked your emotions. Breathe and let the cortisol dump dissipate a little before you make phone calls and yell. Whatever has been dropped or missed has been dropped or missed. Move to next steps and when. Never ever assume that the doctor’s office will call you about test results. You make the call and leave a message that you are waiting on results and have not received them yet. Sometimes, you may be told that the office will call you, if anything is wrong. They may mean to, but crap happens. It is your health so you be responsible for calling them.
Have you ever sent an email to someone and waited on a reply. But, you got no reply and now it is a week later. You are mad or disappointed. You either write another email or forget the whole thing. Guess what? They may have never received your first email. It may be in their Spam folder or something screwy may have happened and they did not get it at all. Give them a call and ask.
Don’t assume your texts are going through either. Follow-up with a call. Strange things happen all the time.
Set and keep your follow-up appointments. If you are dealing with chronic health conditions, you may have multiple doctors and will need regular check-ups. Usually, 3 or 4 times a year. These follow-ups are not punishments. They are to keep you healthy and on track to have the best quality of life possible. For follow-ups, you pick your days and time. Maybe Tuesdays are best for doctor appointments. Tell the scheduler, what day you want and what time will work for you and they can search for openings.
See your dentist twice a year too. It isn’t just about your teeth and gums; it is also about heart health. If you have a fear, they have gas.
Get better at describing how you feel and what is going on with you.
Be specific in your descriptions
Focus on how your life is being affected by what is going on. Be specific. Don’t say, I get tired easily. Tell what you are specifically doing. For example, I am having trouble drying my hair with a blow dryer, I feel weak and tired. My back hurts, here (point it out) and describe the pain (achy with movement, dull pain all the time, sharp pain when I do this.) and what makes it feel better and what makes it worse.
Which of the following would be better information? My right knee hurts. OR …My right knee feels like it is giving out and it aches in the evening. In your mind, you know that your knee hurts and you know what you have done and tried. You also know what has worked and what has not worked. You are also concerned that it will give away and you may fall. Your doctor does not know all of this and they cannot read your mind. You have the clues that they need to help make an accurate diagnosis or treatment plan. Maybe, you are having trouble climbing stairs or going down stairs. Describe the trouble and how your knee feels.
Use a metaphor or simile to describe what is going on. Be descriptive.
-
- My legs feel like I am carrying 20-pound weights on each leg as I walk.
-
- This pain feels like I am being stabbed.
-
- I have jackhammers in my head.
-
- My neck feels like rocks grinding together with bits and pieces chipping off.
-
- I am itching so badly, that I wish I could dig my fingernails in and pull out the affected area.
-
- I feel like barbed wire is wrapped around my foot.
-
- My headache is on one side and it is continuous with occasional lightning bolt zaps.
-
- My stomach feels empty and gnawing about an hour after I eat.
Rarely, but it does happen, you have to say… “ I am not right. This is what I have observed and felt.” You may not have any concrete signs or symptoms, but you know that your body is not right. Be observant about your body and how it feels, be observant about your thoughts and what you are thinking.
Things to help you write out your notes for your appointment:
Questions to ask yourself about your symptoms:
-
- What exactly are my symptoms?
-
- Are the symptoms constant? If not, when do I experience them?
-
- Does anything I do make the symptoms better? Or worse?
-
- Do the symptoms affect my daily activities? Which ones? How?
Go through the story in your mind and pick out the relevant information, remember, doctors like bullet points.
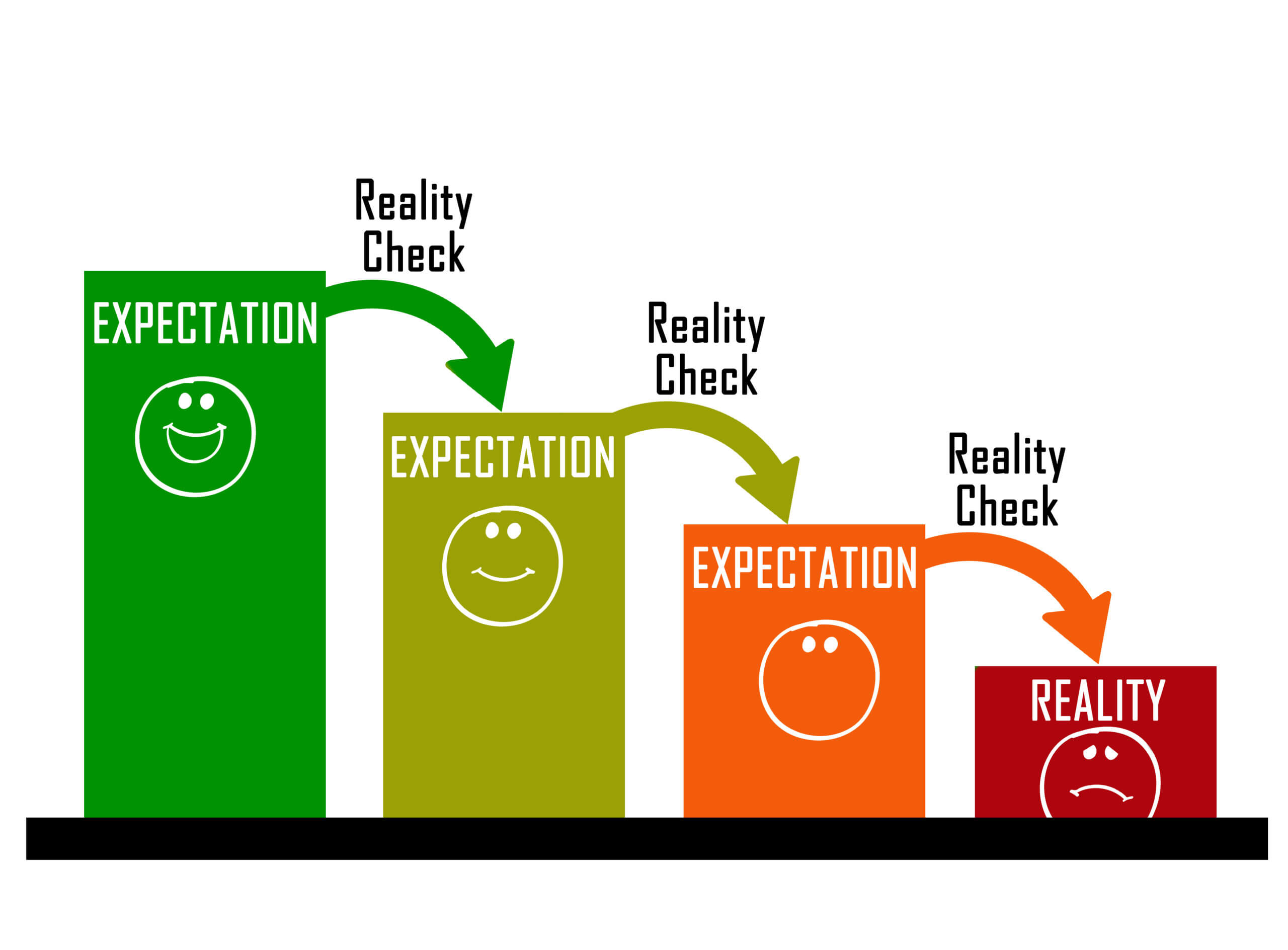
Just because your doctor can’t make a diagnosis does not mean that there is nothing wrong with you. In too many cases missed diagnoses happen. Be persistent about what is going on. Get a second or third opinion.
Missed diagnosis, also called delayed diagnosis or failure to diagnose, means that the medical professional did not realize a medical condition that a patient presented with signs and symptoms of. This may be because the doctor did not recognize a constellation of symptoms that should have prompted them to test for a certain condition, or because symptoms that might indicate a serious condition are also associated with a number of other, minor health issues.
Misdiagnosis means that a person with one medical condition was diagnosed by a doctor with another condition that they do not have. In the best-case scenario, a misdiagnosis results in a little frustration and the waste of some time and money. In the worst-case scenario, the treatment for the wrong condition could further sicken or kill the patient, or delay diagnosis of the true condition until it is too late for it to be successfully treated.
Common missed diagnoses and misdiagnoses in women:
-
- Autoimmune diseases (there are about 100 of these and too often the symptoms are not specific enough and you may be labeled a chronic complainer)
-
- Polycystic ovary syndrome
-
- ADD (attention deficit disorder) & ADHD (attention deficit and hyperactivity disorder)
Common missed diagnoses and misdiagnoses of men:
-
- Obsessive compulsive disorder
Be diligent regarding your own health. You are not crazy and you are not a hypochondriac (well, most of you aren’t). Be as factual as you can be and understand that you have the clues. Get your symptoms across to your healthcare provider. Have the care recipeint be as involved as possible with all appointments.
Pat