How caregiving is like working out, rest days are important.
April 13, 2022
Why is it okay to take a rest day or two from working out but, it is not okay to take a rest day from caregiving responsibilities or helping your loved one? Think about that. We have the research and the information about listening to our bodies. That rest days are just as important as workout days. That if you cannot mentally concentrate on a lifting day, you are better off skipping that workout. If you push through your chances of injury are greatly increased. Then what? You got it… you will have to take four to six weeks off to heal.
Helping out a loved one is the same kind of thing. Sometimes it is mentally exhausting and sometimes it is physically exhausting. You know that you need a break, but will you take a break? Will you push through? For how long? At what cost to you and your own health?
When you are a caregiver for more than 3 months
These are things that all of us need to think about. The problem is that we don’t think about these things. We just jump in and do. That is great, if it is for a short time. The problems arise after we have been helping for a longer period of time. Three to six months is what I consider a longer period of time. At about 18 to 24 months burnout has begun, if you have not gotten help or taken time outs.
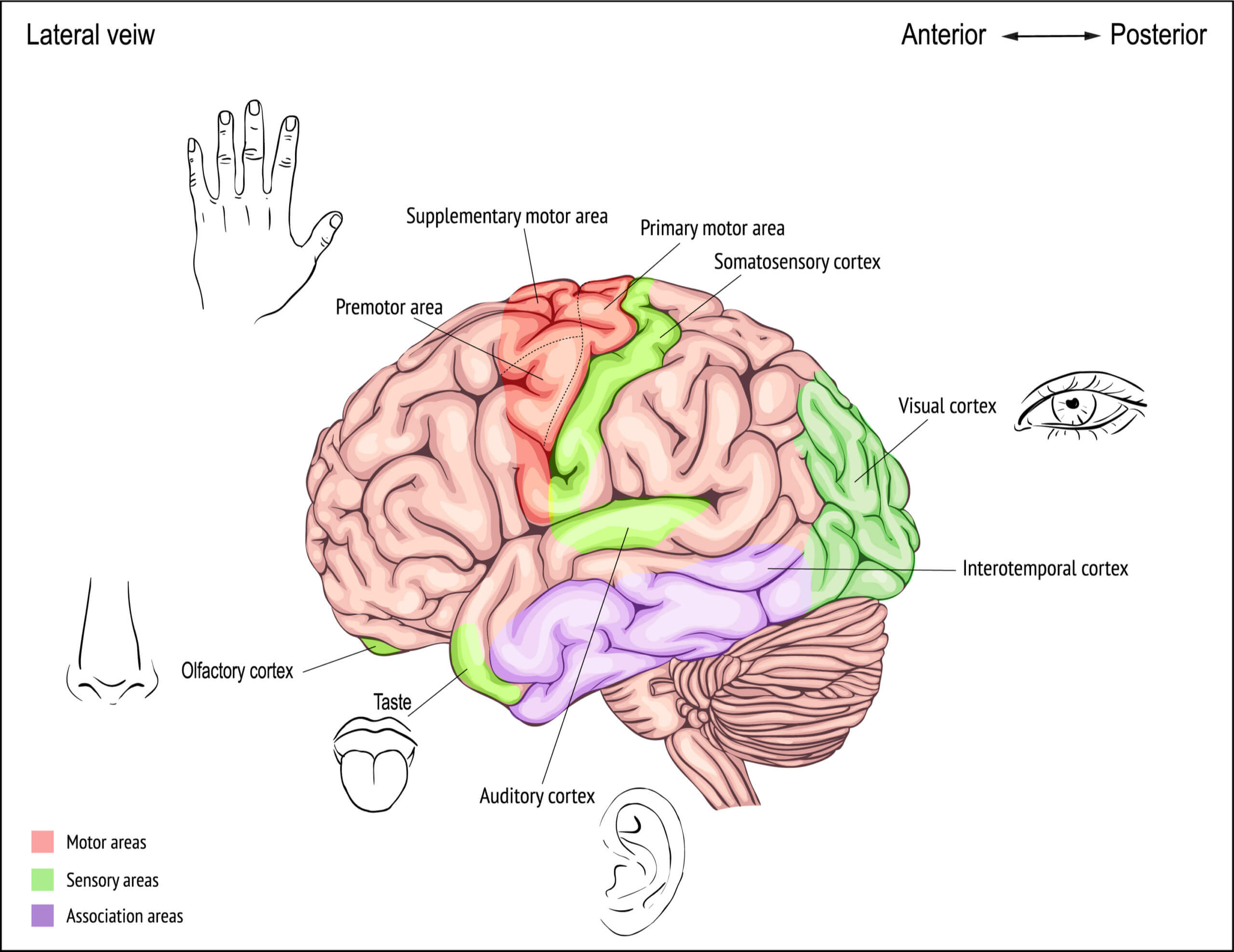
I get it. It is hard when you are in the big middle of things to think about what would be best for all involved. You get in to survival mode and you just do. Some of us don’t want to think about what would be best for us and for out loved one. Thinking is hard and it takes a lot of energy when you are learning new things or doing new things. Remember, you only have about three hours of focused energy per day to use. When are your good hours? When are you able to concentrate and work on detailed projects the best? The rest of the day, you can do the things that do not take as much mental energy or focus.
Habits improve our health and well-being
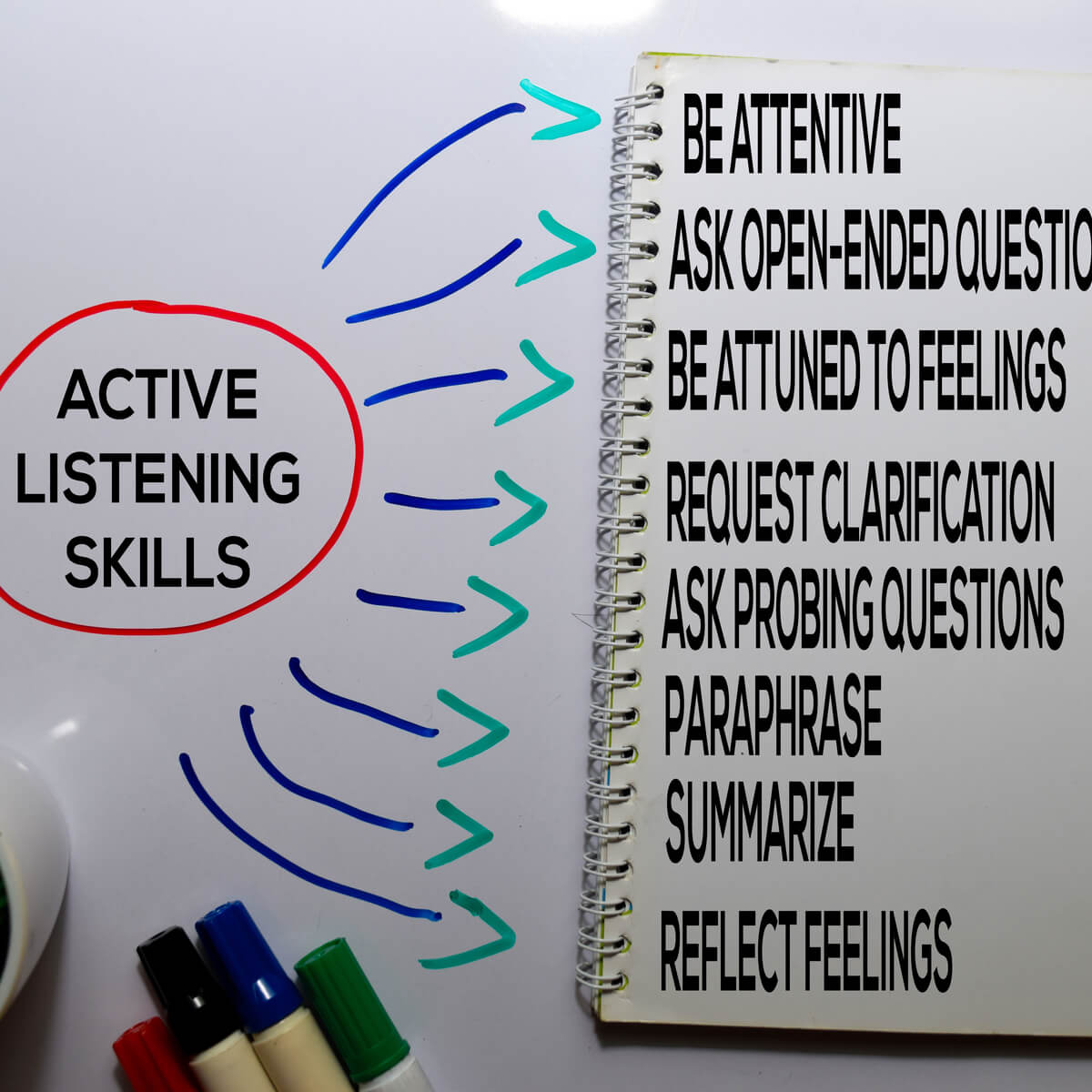
Developing habits are good for us. I am talking about positive habits. They decrease the expenditure of mental energy. Basically, when we have habits, we do them and we do not have to waste any mental energy or focus to think about the “who, what, when, where, why” things. We just do. We have already learned. Some folks call it discipline and others call it a routine. The demands of caregiving are exhausting physically and mentally.
The dreaded where to go when eating out question…
As with most of us, the most aggravating thing is trying to figure out where to go for dinner. How much time and energy is wasted on this simple act? We ask each other, “Where would you like to go?” The reply is usually, “I don’t care, where do you want to go?” Yes, you know what is coming next. “How about the Roadhouse, you ask?” Wait for it …. The reply is … “I don’t want to go there.” Here comes the hard part … do you say this or just think it? “Obviously, you do care. So, where do you want to go?” The back and forth continues, until finally a place is chosen. How do you feel after this discussion? Tired? A little miffed? Wondering why it is a chore to pick a place to eat? Sometimes, you can give them three options and they still do not like any of them. But, they don’t have any options to give you. Why is that? Sorry about that, I digressed.
How does the rest of your evening go? If both of you can let it go, the evening will probably be okay. If one or both of you do not let it go, then chances are you will not be having pleasant conversation the rest of the evening.
I wonder how much better and easier it would be if one of us said, from the beginning, “I would like to go to the Roadhouse, do you want to go?” The other person can say yes or offer another suggestion. Then the suggestion could be taken or not and they can go or stay at home. Shoot, one person gets to pick this time and next time the other person gets to pick.
We are trying to get a consensus, but sometimes that is not possible. The same thing happens when you are a helper or care giver. You may or may not get a consensus. A “good enough” decision has to be made. NOT perfect. Progress, not perfection is what we are after.
If you do not have habits or routine, try this for two weeks and see how you do and how you feel. Plan your breakfast every day. It does not matter if you eat at home or go and pick something up. Figure out what it will be the night before. Pick out your clothes and shoes the night before. Stick to this routine for two weeks.
Hopefully, you will find that having a routine frees your mental energy for other things. What day or days do you clean the house? Do laundry? Change the sheets? Workout? Run or walk? Schedule them like an appointment, until they become a habit. When they become a habit, the less focused mental energy you will use and will have that energy to do other things. Learning to manage your energy is much more efficient than managing time.
Which of these fits you today?
8 SIGNS YOU NEED A REST DAY
1. YOUR RESTING HEARTRATE IS ELEVATED
2. YOU FEEL TIRED
3. YOU’RE MOODY
4. YOU FEEL SICK
5. YOU’RE ALWAYS SORE
6. YOU’VE HAD A FEW BAD WORKOUTS IN A ROW
7. NOTICE YOU’RE NOT GETTING ANY STRONGER
8. YOU FEEL THAT YOU NEED A REST DAY
From Tough Mudder https://toughmudder.com/blog/no-excuses/signs-need-a-rest-day/
14 Signs you need a rest day from being a helper or care giver
-
- Feeling “trapped” or hopeless
-
- Losing patience or compassion for your loved one
-
- Overreacting to small accidents
-
- Resenting or neglecting your loved one
-
- Withdrawing from your personal hobbies and friendships
-
- Oversleeping or not sleeping enough
-
- Overeating, not eating enough, or eating a lot of high-sugar foods
-
- Having health problems
-
- Abusing drugs or alcohol
-
- Having thoughts of suicide
-
- Making mistakes
-
- You are irritable
-
- Signs and symptoms of depression
-
- You feel exhausted most of the time
I can’t say it any better than Daily Caring has said it in their article.
6 WAYS TO MAKE IT EASIER FOR CAREGIVERS TO TAKE A BREAK
1. Accept that you’ll feel guilty
Guilt is a normal part of caregiving simply because you care – it’s never going to disappear.
Don’t let this stop you from getting the caregiving help you need.
Taking regular breaks is the best way to maintain your overall health and your ability to provide care.
Besides, how good would you feel if you never took any breaks and your health declined to the point where you could no longer care for your older adult?
It doesn’t do them any good if you’re not physically or mentally well enough to be their caregiver.
2. Don’t ask your older adult for permission
This isn’t a decision that your older adult gets to make.
Many older adults refuse outside help because they’re uncomfortable with the idea.
And someone with dementia doesn’t have the cognitive ability to make a rational decision.
When seniors refuse, they’re not thinking of your needs and are often not considering their own true needs either.
That’s why you need to make the decision, regardless of how they feel about it.
All that matters is that they’re safe and well cared for when you’re not there.
3. Start before you really need it (if possible)
It may take some time to find the right person to help and for them to learn the caregiving routines.
That’s why it’s helpful to find help before you really need it.
When you’re putting together a team of family, friends, and volunteers, it can be less stressful if you have some time to get the team in place and work out the details.
To make the transition easier, you could have someone come and shadow you until they learn the ropes and can be left alone with your older adult.
Or, you could have someone come for a short time in the beginning and gradually increase their time as everyone adjusts to the new situation.
4. Combine paid services with help from friends, family, and volunteers
Hiring caregiving help can be expensive. But even if the cost is high, maintaining or improving your health is worth it.
Being open to different sources of help also lowers the cost of taking regular breaks.
Ask family or friends for help and seek out local volunteer programs that offer companionship services.
Then supplement those hours with paid help as needed.
5. Check in to know that your older adult is well-cared-for
You might be afraid or nervous to leave your older adult with a stranger or a family member with limited experience.
To give you greater peace of mind, use simple, discreet ways to keep an eye on them and make sure they’re treating your older adult well.
You could sometimes come back early as a surprise check-in to see what’s been happening.
Or while you’re out, call occasionally to hear how things are going.
Another good move is to ask the caregiver to take notes so you’ll know what happened while you were out.
6. Be creative when introducing the hired caregiver
Nobody wants to be told that they’re getting a babysitter.
If your older adult is very resistant to outside help, be sensitive and creative when introducing them to the household.
A careful approach is especially important to prevent seniors with Alzheimer’s or dementia from reacting with fear or anxiety.
For example, you could introduce the person as your helper around the house and have them help you with meal prep, light housekeeping, and simple care tasks.
After a few of these visits, it will seem normal that they’re around and it will be easier for you to leave to “run errands.”
You could also position it as doing that person a favor. Perhaps you could say that this person is in need of extra income, so you’re helping them out with a few hours of work here and there.
If family or friends are helping, you could say that they wanted to visit and spend some time catching up. When they become regular visitors, you can start popping out to “run errands.”
By DailyCaring Editorial Team
Pat