When you are frustrated, upset, or angry, you cannot problem-solve very well.
Guess what part of your brain is hijacking your normally calm, cool and collected self? The friggin’ amygdala is at it again. Fight, flight, freeze or fawn stuff. Those are the only options that we see when our amygdala is activated.
July 20, 2022
Friggin’ Amygdala and the Problem-solving Process
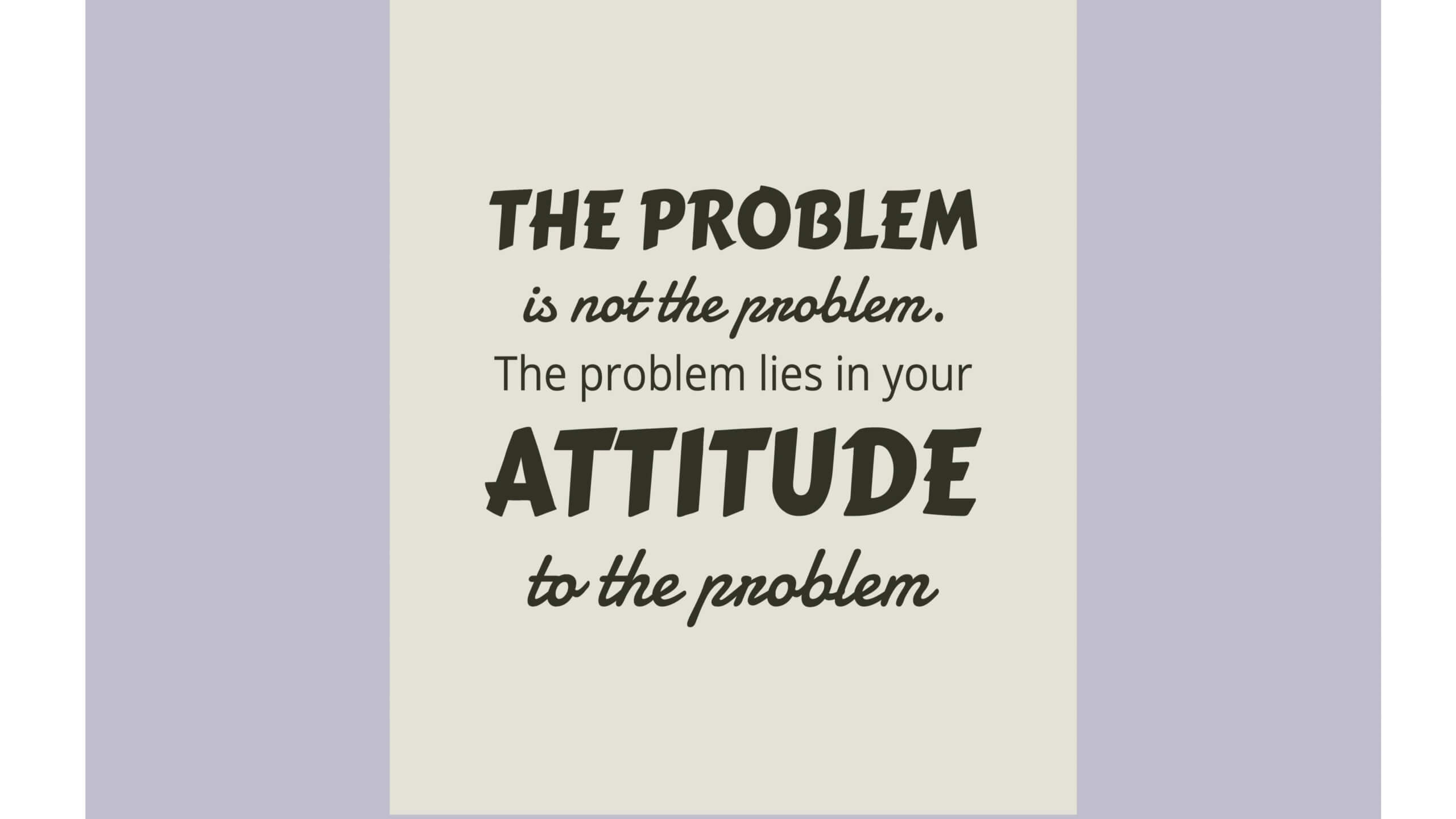
We know that the amygdala hijacks our abilities to make good decisions and lowers our ability to problem-solve because we cannot think about our true options. What about our attitudes? I am having a little trouble explaining attitude, so bear with me here. We each have assessments or judgments about “attitude object” We use words to describe what we like or do not like. Examples include, Like, prefer, love, do not like, hate, can’t stand, etc. We make these statements in relation to ourselves. “I like _____.” “I hate ____.” Attitudes are really evaluations that we make based on what is important to us. Our experiences are different and so our attitudes may be different too.
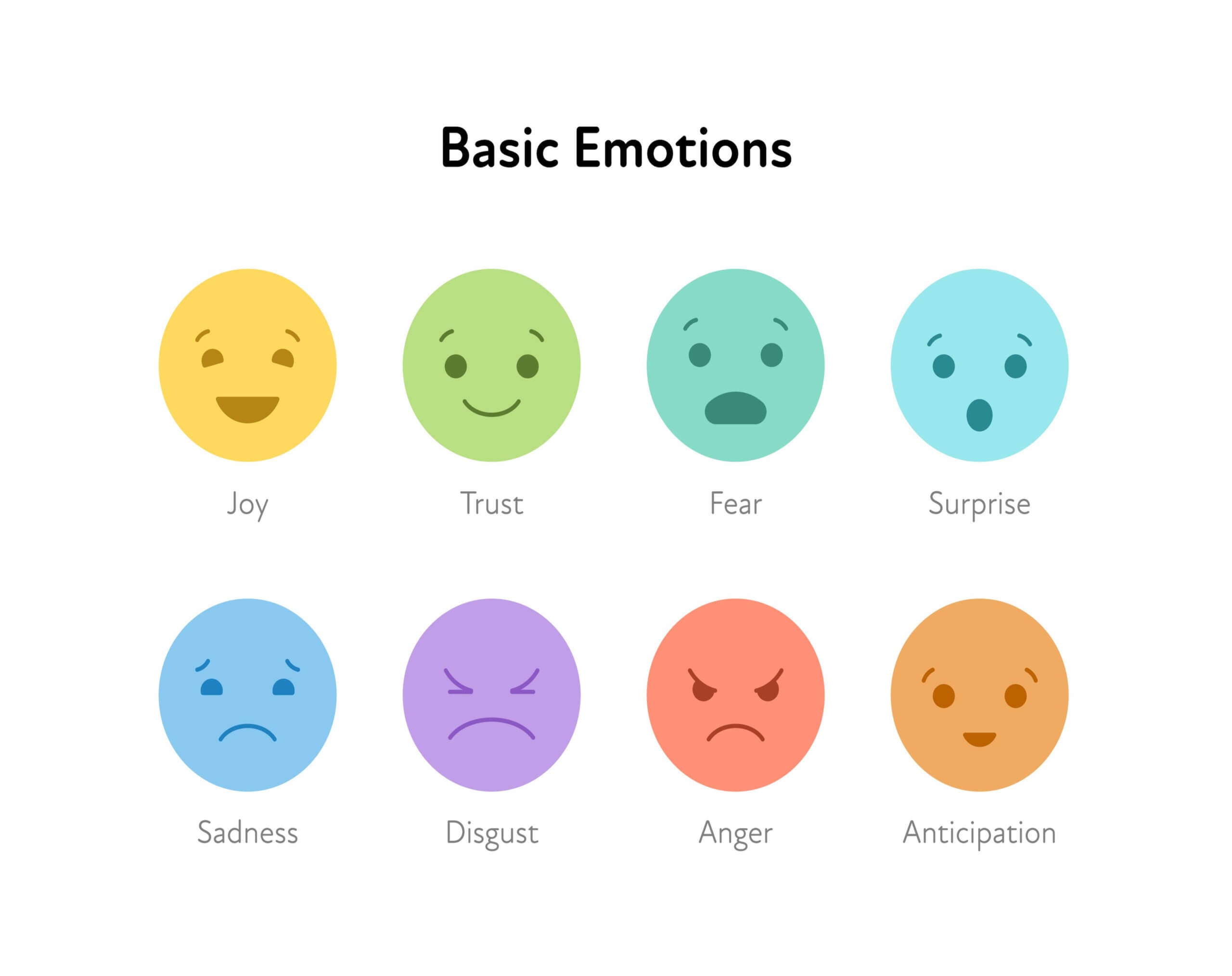
Attitudes are shaped by feelings and emotions. And another tidbit, emotion is sometimes the driving force behind our attitudes and behaviors.
There will be some things that you feel very strongly about. There will also be things that you don’t feel strongly about.
Structure of Attitudes
Attitude’s structure can be described in terms of three components.
-
- Affective component: this involves a person’s feelings/emotions about the attitude object. For example: “I am scared of spiders”.
-
- Behavioral (or conative) component: the way the attitude we have influences on how we act or behave. For example: “I will avoid spiders and scream if I see one”.
-
- Cognitive component: this involves a person’s belief/knowledge about an attitude object. For example: “I believe spiders are dangerous”.
This model is known as the ABC model of attitudes.
Does a negative attitude affect problem-solving skills?
A negative attitude towards a problem makes it worse. When you think negatively, it only magnifies and deepens the emotional weight of “said problem.” You not only see the problem as a problem, you see it as an enemy or an attack on you. You can become overwhelmed and paralyzed. You know what comes next, don’t you? The downward spiral. Which makes the attitude and the problem much worse?
I like the Fish! Philosophy and want to share a little with you.
The FISH Philosophy to help problem solve
The FISH! Philosophy doesn’t promote “correct” or “approved” attitudes over others. Every situation is unique. But it is important to mindfully Choose Your Attitude. You may not control what happens to you, but you do get to decide how you respond to it.
Making a conscious choice isn’t easy, especially when a situation hijacks your emotions and drives you to react the same way you have hundreds of times before. It takes practice to take control of your response, instead of letting it control you.
Here are four tips to help you take charge and Choose Your Attitude:
1. Be aware of your inner voice
External events may trigger your feelings, but only after they go through an internal filter called your inner voice. Your inner voice starts talking to you as soon as you wake up, issuing opinions about everything you see, hear, touch, smell and feel.
Your inner voice is rarely a neutral observer. It judges each experience through the likes and dislikes you have accumulated over a lifetime. It looks for evidence that you are right and the other person is wrong. It exaggerates how bad the situation is or imagines how it might go off track. Sometimes it puts other people down. Often it puts you down, questioning your talents and capabilities.
If you want to choose your attitude, not just react, you must challenge your inner voice. Catch it in the moment, then take a step back. Instead of just accepting what it is telling you, observe it as a neutral onlooker.
Just becoming aware that it is a voice, and what it is saying is one of several possible interpretations, helps you decide how much to believe it—and the best way to respond.
2. What’s your goal?
To mindfully choose how you respond to what life throws at you, you need a plan. Decide who you want to “be” today. Keep your goal top of mind. Select a few words that describe your intentions, such as “patient”, “open” or “helpful”. Focus on living those qualities.
Moment-to-moment awareness is key. Ask yourself throughout the day, “What is my attitude now? Is it helping me to be as effective as I can be? Is it helping the people who depend on me?”
Think ahead: What people or situations are likely to test your attitude today? What might push your buttons? Rehearse how you will respond. Reaffirm your goal and stay focused on the response that helps you achieve it.
Consider the long-term consequences of your reactions. Say a member of your team makes a bad mistake or you have a disagreement with them. Is the momentary satisfaction of tearing into them worth damaging your relationship? Disagreements and problems come and go, but your relationships are not so easily replaced.
3. Adopt a “growth” attitude
Your attitudes are shaped by how you see others—and by how you see yourself.
People with a “fixed” attitude see their abilities as set and established. They know what they’re good at and view what they’re not good at as talents they don’t have the capacity to improve (“I could never learn that!” or “I wasn’t born with a brain for that!”).
People with a fixed mindset see tasks requiring them to step outside their comfort zones as threats. Confident in what they already excel at, they fear mistakes that might threaten their identity. They only pay attention to feedback and information that confirms their beliefs.
People with a growth mindset believe they can always improve their skills. It doesn’t mean you can do anything, like play in the NBA or be an opera star. It means you never know what more is possible for you and do not limit yourself before you try. It means seeing mistakes as a chance to learn and stretch yourself.
Studies show people with growth attitudes are more engaged and empowered. They handle change more successfully. They’re more flexible and open to seeing new solutions. In workplaces that support a growth attitude, people collaborate more and feel safe to try new approaches.
4. Challenge your assumptions
It’s natural to assume the worst about other people’s motives and capabilities, especially if we don’t agree or connect positively with them. Believing they offer little of value to us, we usually try to avoid them—which doesn’t do much for team collaboration and camaraderie.
If you have a coworker or employee you think has a bad attitude or lack of motivation, move past your assumptions. Reach out. Find out why—not with accusations but with caring questions. You may learn they are dealing with a trying situation at home or work stresses you didn’t know about. Knowing this will help you respond to them more productively.
Treat them with a little kindness and encouragement and you may see a different side of them. Learn their perspective. Find out what they do well and seek their input. People tend to respond to you based on how you treat them. If not, you have chosen an attitude you can be proud of.
Back to problem-solving.
If you don’t see a problem as a disaster, you are more likely to be calm and think about your options. Are you open to looking at the problem as an opportunity? We like opportunities. Our brains like opportunities. Our brains like to brainstorm. Finding any and all possible solutions to our dilemma. Now, not everything thing will be a winner, but the whittling down comes a little later in the process.
Improve problem-solving skills
Would you like to be a more effective problem-solver? Then invite positivity into your environment. Positive attitudes increase creativity and problem-solving skills. A positive attitude also increases productivity.
-
- Some ways to create a positive attitude:
-
- Write down three things you are grateful for each day (not the same 3 things, either)
-
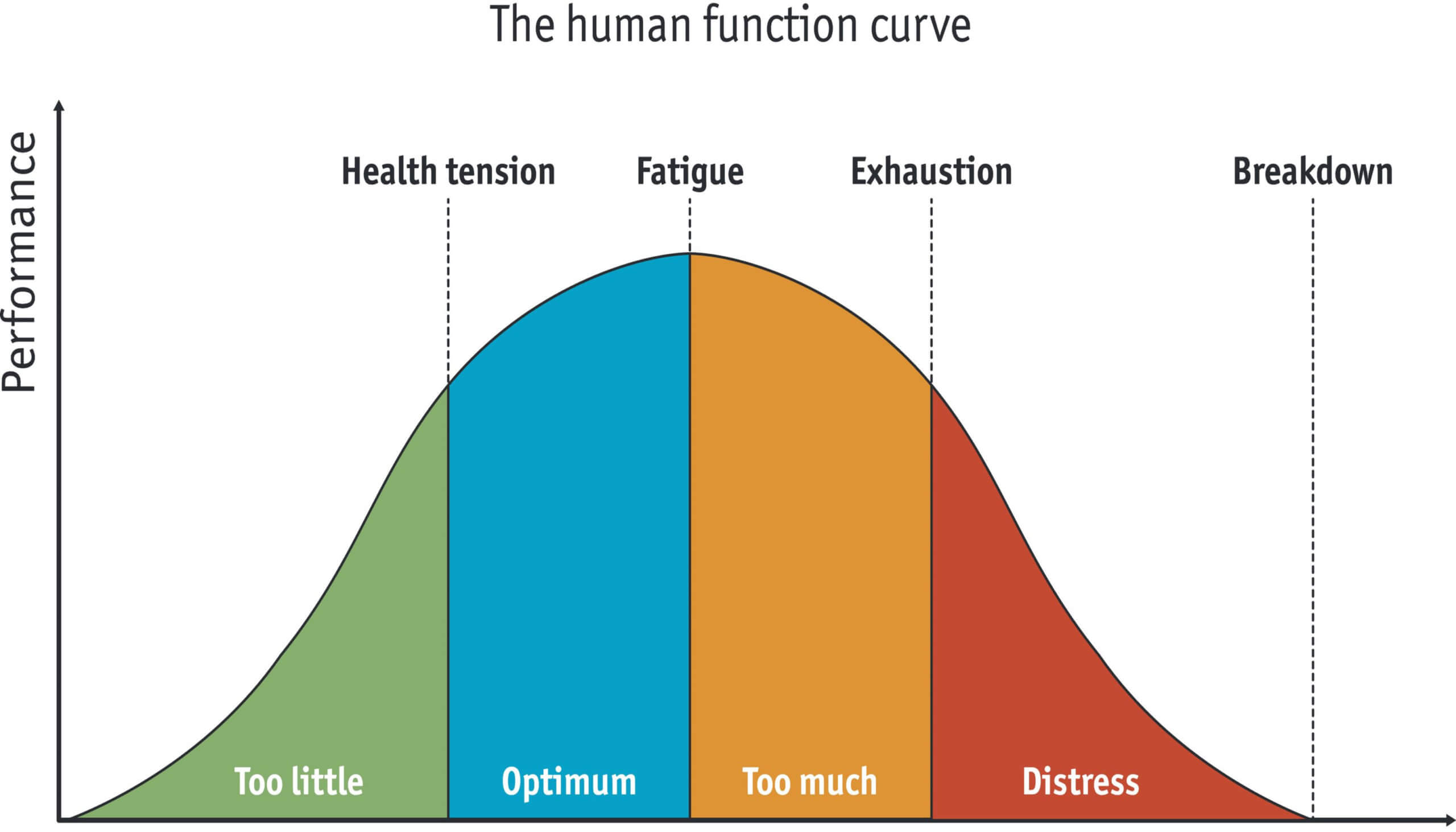
- Take breaks during your day
-
- Tell a few jokes, or watch a funny animal video
-
- Think about the ways to have a great morning and do them
-
- Don’t spread gossip, don’t listen to gossip
-
- Look forward to something outside of work
-
- Practice meditation, walk, work-out
-
- Have some “you time”- unwind, destress, play
-
- Listen to music, watch a funny TV show, read an uplifting or funny book
-
- Hang-out with positive people
-
- Stop the “stinking thinking”
-
- Sit with your feelings and acknowledge them
-
- Assume responsibility, choose your response
Pat