I have seen both ends of the spectrum. I have seen the complete breakdown and fights between siblings trying to help their mom. I have also seen the absolute success of siblings working together to take care of their dad.
Why can one family make it work and another family implode?
June 8, 2022
You know people that can put the “fun” in dysfunction. It can be amusing when the stakes are low. What happens when the stakes are high and everyone needs to do their part? It’s not so funny then. It is downright hard and very stressful.
Family dynamics, sibling relationships, parent-child relationships, rivalries, blended families, issues from the past, issues from the present, etc. Relationships can be complicated. Relationships can be messy. There may not be a relationship anymore.
First, you need to decide if you want to help your mom or dad. No judgement here, I have heard the stories of how you were treated as a child by your mom. I have heard the stories of what you endured as a child and how you worked hard to get out of that situation. No one is required to help or provide assistance to their mom or dad. It was usually one or two of the kids that had to endure the hell. The other children were spared. This is also where you and your siblings will disagree about what happened in the past. We can only speak about our own experiences and perceptions.
The first time that I heard of people being mistreated or abused when they were kids, it was hard for me to imagine. I had no reference point for that. My brother and I knew that we were loved and wanted. We got spanked, but we were never abused. You don’t know what someone else has been through. It is always hidden and it is never talked about. Why was it so hard for me to imagine? Because, I could not imagine my mama or daddy doing to me what other parents did to their kids. After hearing about others being slapped, locked in their room or being starved, you start to realize that not everyone grew up like you did.
For some of these kids, they did not admit it to themselves until they were in their 30’s or 40’s and it is not easy for them to talk about. I get why some folks cannot or will not help to take care of their parents either from a distance or hands-on care. Your own safety and mental health needs are absolutely of paramount importance.
The other things that we need to look at are the siblings that do not want to help because they don’t want to help. They have no real reason other than it will affect their own lives. Tough toenails, sometimes you have to do things that you don’t really want to do. It is called being an adult. Don’t misunderstand me, I am not saying that you have to do the hands-on care, but you do need to be involved in seeing to their care. See, right there, I used my own feelings and my own background with my own family to make a generalized statement about caring for a loved one. I apologize to you for that. I don’t know your experiences and I respect your decisions.
For this article, I am assuming that you have siblings and you do want to help your mom or dad. You do love them and you do care, you may not know where to start or what to do first. Safety is of paramount importance. Are they safe? Are they in a safe environment? Do they have nutritious food and are they eating? What about drinking their water every day? Taking their meds appropriately? Showering/Bathing and keeping up with their personal hygiene? Are they putting on clean clothes or are they wearing the same thing every day? What are their limitations? Are they physical limitations, mental limitations or a combination of both?
It seems as though there is always a primary caregiver and then supporting caregivers. All of you may be hands-on helpers or a combination of hands-on and have in-home help. Being a caregiver or helper is hard. It is demanding, frustrating and tiring. Not everyone is good at being a hands-on caregiver. But, they can be great at other things.
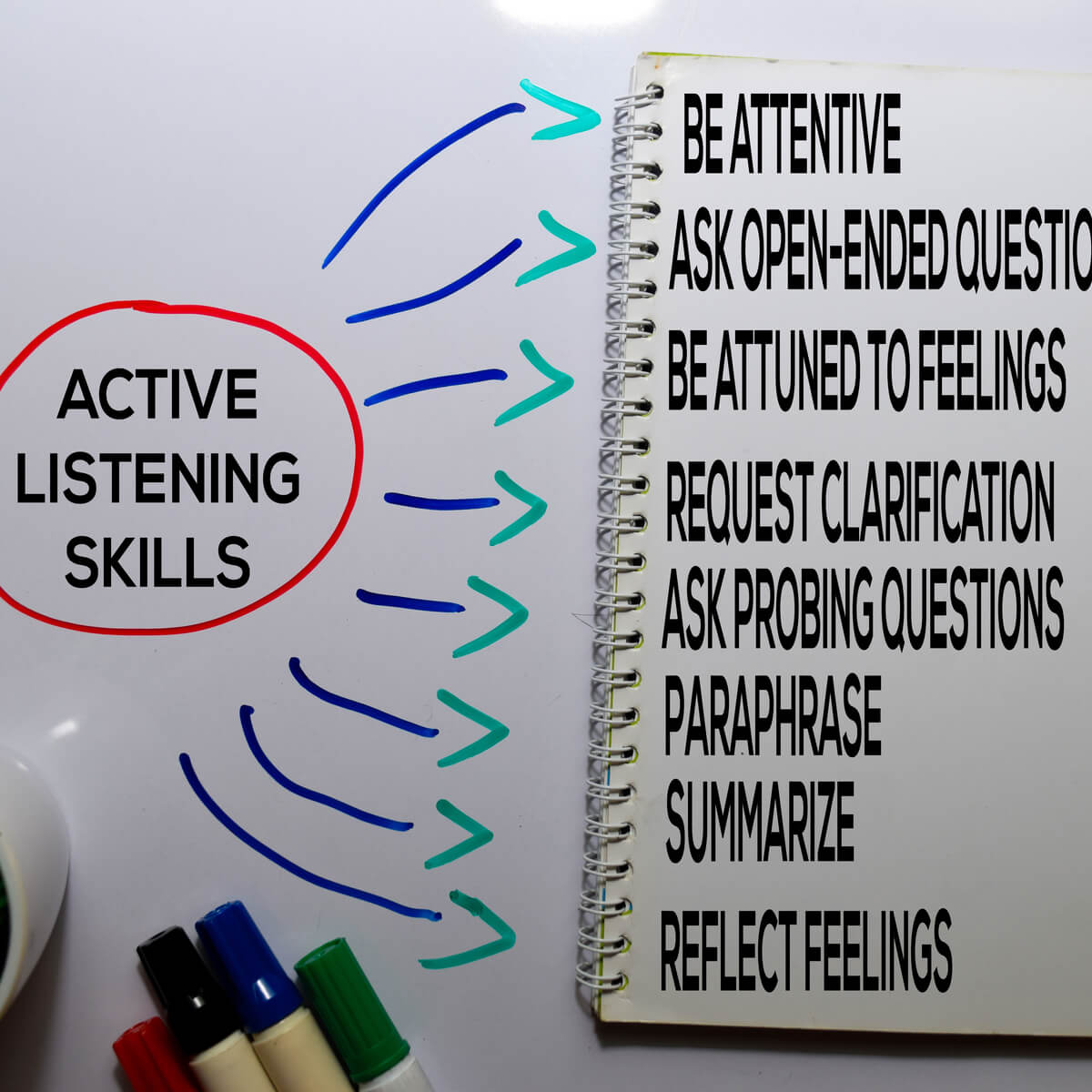
Communi-friggin-cation is the key. You have to talk to each other. You have to work out a schedule. You have to figure out what your strengths are and what you are willing to do and what you are not comfortable doing. Maybe, you are good at doing most everything but personal hygiene tasks. Maybe personal hygiene tasks are okay with you, but you hate cooking and doing the laundry. Maybe your mom or dad needs help getting up out of bed or a chair. Do you know how to help them safely? You probably need training in how to lift and transfer them safely.
What happens when one sibling see things differently than another sibling with regards to where the parent is exactly “at” in their disease progression? De-Nile (denial) ain’t just a river in Egypt. When you cannot agree, it is time for a frank discussion with a social worker, their physician or me. Why would I say to meet with someone rather than tell you to roughshod over your sibling? Remember, your parent may tell one sibling one thing and something different to another. It is usually not malicious. They are trying to keep up appearances that they are okay.
A neutral third party can be objective, so that you and your siblings have a better understanding of where your loved one is, right now and also, what is to come. It is hard. We call it the practice of medicine, because there are no absolutes. We make the best decisions that we can with the information that we have right now. As the status or information changes we will make adjustments.
Some of you are thinking, but my sister is a looney tune. Others are thinking, my brother is the baby of the family and is no help at all. Other complaints include – My sister is a know-it-all and a martyr. My brother lives out of state and thinks everything is fine. All my sister/brother wants is for them to die and get their money. My sister and I don’t get along. You may even hear, “I can’t bear to see mom/dad like that.” There is some kind of hurt or conflict in the sibling relationships.
If you love your mom or dad and want the best for them, then do what is best for them. Keep that your main goal and focus. You have compartmentalized before; you can do it again. You will get distracted and you will harp on your sibling(s). When you start griping and yelling about what “they are doing or not doing,” maybe it is time to refocus on the goal.
Have the roundtable discussion. Keep the main thing the main thing. Decide who will do what and by when. Calendar it. Place the calendar on Google Docs so everyone knows what is happening. Include your triggers for when it is time to bring in paid help. Of course, you need to figure out how and who is going to pay for it. Ideally, it will be from your loved one’s money or a long-term care insurance policy, but that is not always an option. Can the siblings pitch in money to help? Some can and some cannot. Be upfront about what you can and cannot contribute financially and time wise. You can make a plan when you know who and what you have to work with. You are looking for progress, not perfection.
Clues That You Are Acting out of Emotional Needs or Fighting Old Battles
- Your level of emotion is out of proportion to the specific thing being discussed right now. For example: getting into a heated argument about which of you should go to the doctor with Dad next week.
- You or your siblings criticize the way you think another person is being, for example: selfish, bossy, uncaring, irresponsible, or worse.
- You feel that none of your siblings understands what Mom needs the way you do and you are the only one who can do certain things.
- You or your siblings generalize a discussion, saying, for example, “You always do this!”
- You or your siblings criticize the way one another feels, for example, “You don’t care anything about Mom.”
Here, I stole this from Family Caregiver Alliance.
Tips for Winning More Support from Your Siblings
- Try to accept your siblings—and your parents—as they really are, not who you wish they were. Families are complicated and never perfect. There are no “shoulds” about how people feel. They are not bad people or bad children if they don’t feel the same as you do. If you can accept this, you are likelier to get more support from them, or, at least, less conflict.
- Do not over-simplify. It’s easy to assume that you are completely right and your siblings are all wrong—or lazy, irresponsible, uncaring, etc. Each person has a different relationship with your parent, and each person’s outlook is bound to be different.
- Ask yourself what you really want from your siblings. Before you can ask for what you want, you need to figure this out, and that’s not always as simple as it seems. First of all, ask yourself whether you really, deep down, want help. Many caregivers say they do but actually discourage help. So, think hard. Do you want them to do certain tasks regularly? Do you want them to give you time off once in a while? Or do you feel you have everything under control but you’d like them to contribute money for services or respite?
- Or—and this is a big one for many caregivers—do you really not want them to do anything but you’d like more emotional support? Many caregivers feel lonely, isolated, and unappreciated. If you’d like your siblings to check in on you more, ask them to call once a week. And tell them it would really help if they would say “thanks” or tell you you’re doing a good job. They are more likely to do this if you don’t criticize them for what they are not doing.
- Ask for help clearly and effectively.
- Asking is the first step. You might ask for help by saying: “Can you stay with Mom every Thursday? I have to get the shopping done for the week and it gives me some time to myself.” Don’t fall into the common trap of thinking, “I shouldn’t have to ask.” Your siblings may assume that you have everything covered so they don’t recognize the added responsibilities and “burden.” They are involved with their own lives and struggles and not so attuned to yours that they can read your mind. Also, if you’re not exactly sure what you want from them, you may be giving them mixed messages.
- Ask directly and be specific. Many caregivers hint or complain or send magazine articles about the hardships of eldercare. But these strategies do not work well.
- Ask for what’s realistic. People get more when they don’t ask for the impossible. So, consider the relationship your sibling has with Mom or Dad and ask for what that person can really give. If your sister can’t spend ten minutes with Mom without screaming at her, don’t ask her to spend time; ask for something that’s easier for her, like doing paperwork or bringing groceries.
- Watch how you ask for help—and steer clear of the cycle of guilt and anger.
- Avoid making your siblings feel guilty. Yes, really. Guilt makes people uncomfortable and defensive. They might get angry, minimize or criticize what you are doing, or avoid you. That is likely to make you angry, and then you will try harder to make them feel guilty. They will attack back or withdraw even more. And round and round you go.
- Sometimes your siblings will criticize you because they are genuinely concerned about your parents. Try to listen to these concerns without judgment and consider whether it is useful feedback. At the same time, be bold by asking for appreciation for all that you are doing—and remember to say thanks back when someone is helpful.
- Be careful of your tone and language when you request something. It’s not always easy to hear the way we sound to others. You might think you are asking for help in a nice way, but if you’re angry, that’s the tone your siblings will hear. And they’re likely to react in unhelpful ways.
- Get help from a professional outside the family. Families have long, complicated histories, and during this very emotional passage, it is often hard to communicate with each other without overreacting, misinterpreting, or fighting old battles. Even the healthiest families can sometimes use the help of an objective professional. People like family therapists, social workers, geriatric care managers, physicians, or clergy can help siblings establish what is real about a parent’s health and needs in order to help distribute responsibilities more equitably. In family meetings, they can help you stay focused on the topic at hand and help you avoid bringing up old arguments.
- Steer clear of power struggles over your parent’s assignment of legal powers. Whether or not you have been given your parents legal powers over finances or health, you need to remember that it is your parent who has made these decisions. If you have your Mom’s or Dad’s power of attorney, be sure to keep detailed records and send your siblings statements about how you have spent Mom’s money. This may seem like a lot of extra work, but record keeping is required by law, and being open will reduce distrust or distortion—and lawsuits. If a sibling has been given legal power, try to accept your parent’s decision and don’t take it as a personal attack on you. Do your best to work with the sibling who has the authority by presenting expenses and bills in black and white. If the sibling who has the purse strings doesn’t cooperate, then bring in a professional to explain your parent’s needs and to mediate. If you are concerned about manipulation, a changed will, or undue influence, contact your local Adult Protective Services.
- Don’t let inheritance disputes tear your family apart. If you feel wronged by the way your parents have divided their money and property, it’s natural to be upset, especially when you are grieving. You may feel that you deserve more because you have cared for your parents. If that’s what you feel, you need to discuss this with your parents while they are alive and can make these decisions. If you suspect foul play by another sibling, then this is the time to consult an attorney or Adult Protective Services.
Yet, research shows that most parents feel a need to leave their estates equally as a sign of their equal love for all their children. When they divide things unequally, it’s often because they are worried that a particular child will be in greater need. Whatever their reasons, remember that it was your parents, not your siblings, who decided this. Think hard before you take your anger or disappointment out on your siblings. They are what remains of your original family, and for most people, this relationship becomes more important after parents die.
The above 8 steps are from Family Caregiver Alliance
Will you agree to operate as a team for the best quality of life possible for your mom/dad? Teams set clear goals and responsibilities for team members. Everyone has a skillset, use the best person for the job. Set weekly calls with an agenda that has 3 things on it. Never more than 3. Focus on the here and now. NEVER start a statement with “you.” Use, “I feel, about a situation. Your bothers and sisters may have different ideas about the care needed. That is good. Talk about it and see if better options arise.
Be fair about the division of responsibilities. When you get off track, go back and focus on your goals for your mom or dad. You did write them down, didn’t you?
Shameless plug – I help families figure out where they are, what they will need in the future, develop an action plan to move forward and guide them.
Pat