Nervous breakdown. What does that really mean? It isn’t used as a medical term or a diagnosis, but we all seem to know what it means. It means a mental health crisis. It means an emotional health crisis. It is also known as a breakdown of your mental health.
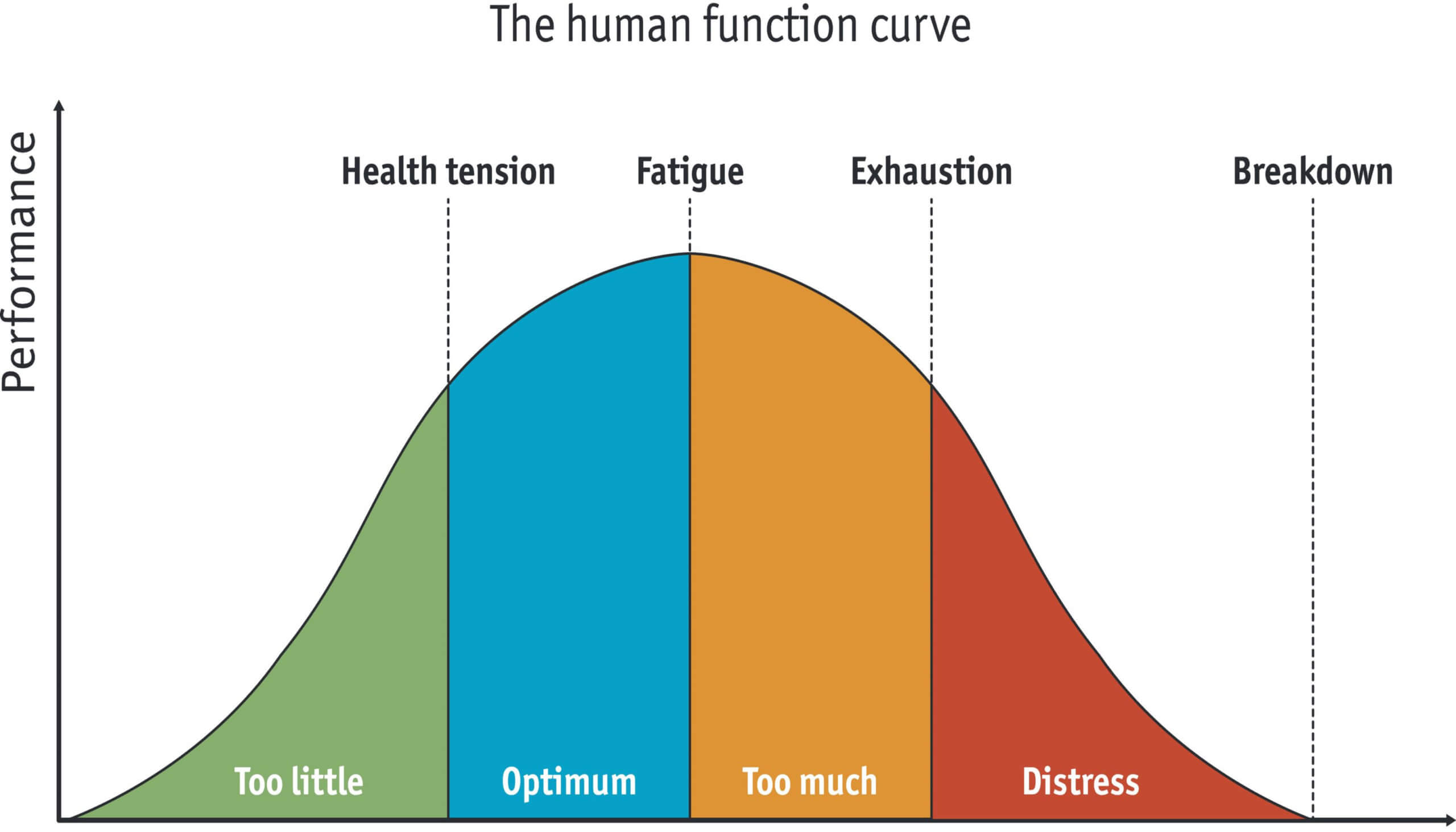
It happens when you have intense physical and emotional stress, with difficulty coping and you are not able to function effectively or normally anymore. You feel like you are losing control. The stress that you are under may have you feeling anxiety, fear, worry, stuck, overwhelmed, and/or nervous. You are at the point where you can no longer function in life. Many caregivers will experience caregiver stress and exhaustion.
October 12, 2022
Everyone’s Caregiver Stressors are Different
Everyone is different and everyone will have different stressors and reactions to those stressors. This is way past burnout.
A few things to watch out for:
-
- You call in sick for a day or two (sometimes, longer).
-
- You miss appointments.
-
- You avoid or back out of social engagements.
-
- You have trouble with healthy eating, exercising regularly, sleep, and your personal hygiene starts slipping.
-
- You withdraw from people and don’t want to leave your home.
-
- You lose interest in things that used to bring you joy.
-
- Panic attacks.
-
- PTSD flashbacks
Things pile on
We all have our own “set point” for a breakdown. Losses are a huge part, especially if they are stacked one on top of another. For example, a death, a divorce, losing your house, a terminal illness, being a caregiver, losing your job, family turmoil, severe financial strain, a chronic medical condition (a worsening chronic medical condition), inability to relax, continued loss of sleep, work stress, school stress, lack of self-care, etc.
As you can see, a lot of things can pile on. Step away, take a timeout! Get a talk therapy appointment, ASAP. You are no longer able to get out of this situation on your own. Breathe, just deep breathe for 5 minutes.
You will have to make adjustments and learn better-coping skills. You will have to learn to say, “No.” You will have to take care of yourself physically and mentally before you can help anyone else. Yes, you can recover, but I want you to be able to prevent burnout.
Burnout is more common. My wish for all of us is that we take better care of ourselves BEFORE we get to this stage. The same stressors apply, they may not be as intense or as long, but they could be.
Burnout is usually defined as chronic stress related to poor life and work practices, that produce exhaustion (physically, mentally, and emotionally). You are overloaded and overwhelmed. When a person is overloaded and overwhelmed with negative emotions and feelings rear their ugly heads. We have hostility, anger, and frustrations and we don’t seem to be able to cope or handle these negative emotions.
Extreme burnout will lead to a mental health crisis.
This article from Medical News Today, explains burnout very well.
Some causes of caregiver burnout include:
-
- Emotional demands: A caregiver can feel emotionally drained, especially if you are aware that the person you are taking care of will not get better despite their efforts. For example, this could happen if a person is caring for someone in palliative care.
-
- Conflicting demands: These are the additional demands a person has outside of their caregiving role, such as looking after children, going to a job, and making time for their partner.
-
- Ambiguous roles: Often, the role of a caregiver is all-consuming. It is easy for a person to lose sight of who they are outside of their caregiving responsibilities.
-
- Workload: Some caregivers may be looking after someone with complex needs. In these instances, it is important a person seeks temporary relief and gets assistance from other carers.
-
- Conflicting advice: In some cases, treatment procedures may change as research progresses. While these changes aim to give people the best care, they can cause a significant amount of disruption and stress if a caregiver has an established routine.
-
- Privacy: Additional clinical support, such as nurses and other healthcare professionals, may visit a caregiver’s home throughout the week. While this can be helpful, it can also take away their privacy.
All of these factors can contribute to a caregiver feeling overwhelmed, self-critical, and drained. If they do not address these feelings, they may start experiencing serious signs of caregiver burnout. Caregiving is both emotional and physically exhausting.
Caregiver burnout can manifest in several ways, and some people may notice they are experiencing some symptoms more strongly than others.
Symptoms of caregiver burnout include:
-
- disrupted sleep
-
- persistent irritability
-
- altered eating patterns
-
- anxiety
-
- increased alcohol consumption
-
- high-stress levels
-
- lack of joy
-
- loneliness
-
- loss of hope
-
- suicidal thoughts
Additionally, symptoms can indicate what stage of caregiver burnout a person is in.
The three stages of caregiver burnout are:
-
- Frustration: A person starts feeling frustrated and disappointed that the person in their care is not getting better. They cannot accept that the person’s condition will decline regardless of how well they look after them.
-
- Isolation: After a while, a person may begin to feel lonely in their caregiving role. They may also grow tired of hearing negative opinions from family members, especially if these family members do not appreciate or recognize the time and effort caring requires. At this point, the caregiver may withdraw from friends and family.
-
- Despair: Eventually, a person may feel helpless and isolated. They can find it hard to concentrate, struggle to find joy in hobbies or interests, and avoid social interactions. The level of care they provide may also begin to drop as they spend less time on their own well-being.
Read the entire article here: https://www.medicalnewstoday.com/articles/caregiver-burnout#symptoms
Pay attention to your signs of stress and aggravation. If you need help or think that you may need some help, give me a call and let’s have a conversation. We won’t know if I can help unless we talk to see.
Pat
865-684-8771 (leave a message, if I am unable to answer)